Macrophage Activation Syndrome (MAS) is a life-threatening hyperinflammatory disorder characterized by excessive activation of macrophages and T lymphocytes. It is considered a severe complication of systemic autoimmune diseases, particularly systemic juvenile idiopathic arthritis (sJIA) and systemic lupus erythematosus (SLE). MAS belongs to the spectrum of hemophagocytic lymphohistiocytosis (HLH) and is associated with cytokine storms, leading to severe organ damage.
Causes and Risk Factors
MAS is often triggered by infections, autoimmune disorders, or genetic predisposition. Some of the primary causes include:
- Autoimmune diseases: sJIA, SLE, Kawasaki disease, and adult-onset Still’s disease
- Infections: Viral (Epstein-Barr virus, cytomegalovirus), bacterial, fungal, and parasitic infections
- Genetic mutations: Mutations in genes such as PRF1, UNC13D, and STXBP2 linked to familial HLH
- Malignancies: Certain leukemias and lymphomas
- Medications: Immunosuppressants and biologics that alter immune responses
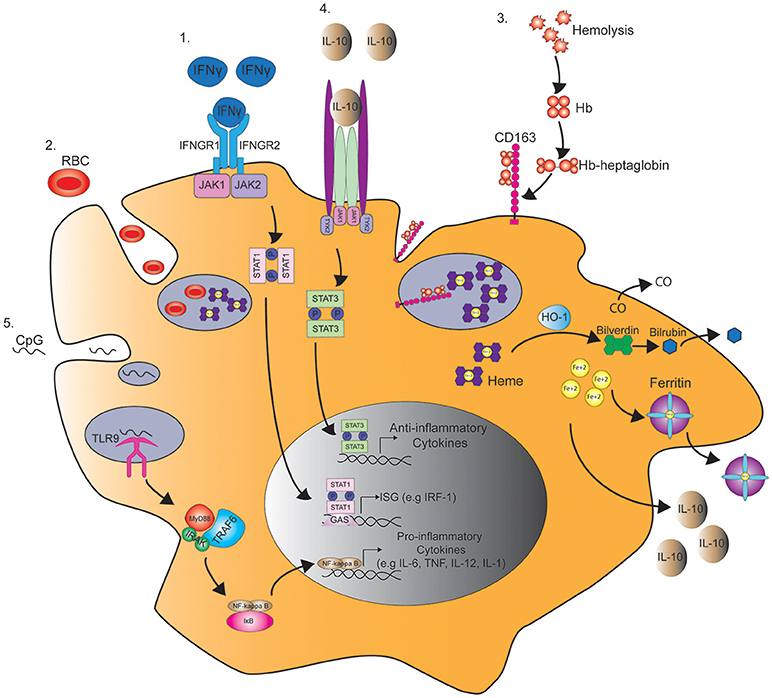
Pathophysiology of MAS
MAS occurs due to uncontrolled activation of macrophages and cytotoxic T cells, resulting in excessive cytokine release, particularly interleukin-1 (IL-1), interleukin-6 (IL-6), interleukin-18 (IL-18), and tumor necrosis factor-alpha (TNF-α). This leads to hemophagocytosis, severe inflammation, multi-organ failure, and life-threatening complications.
Signs and Symptoms
MAS presents with a wide range of systemic symptoms, including:
- High Fever: Persistent and unresponsive to standard treatment
- Cytopenia: Decreased levels of white blood cells, red blood cells, and platelets
- Hepatosplenomegaly: Enlargement of the liver and spleen
- Neurological Symptoms: Confusion, seizures, or coma
- Coagulopathy: Bleeding tendencies and disseminated intravascular coagulation (DIC)
- Elevated Ferritin Levels: Hyperferritinemia is a hallmark of MAS
- Liver Dysfunction: Elevated liver enzymes and bilirubin levels
- Acute Respiratory Distress Syndrome (ARDS): Severe lung involvement leading to hypoxia
Diagnosis of MAS
Early diagnosis of MAS is critical for improving survival outcomes. Key diagnostic criteria include:
Laboratory Findings
- Elevated serum ferritin (>10,000 ng/mL)
- Cytopenia affecting at least two blood cell lineages
- Elevated liver enzymes (AST, ALT) and bilirubin
- Increased soluble CD25 (IL-2 receptor alpha)
- Decreased fibrinogen and prolonged clotting times
- Elevated triglycerides and lactate dehydrogenase (LDH)
- Bone marrow biopsy: Presence of hemophagocytic histiocytes
Diagnostic Criteria (MAS in sJIA – 2016 EULAR/ACR Guidelines)
A patient is classified as MAS-positive if they meet five of the following criteria:
- Fever ≥39°C
- Ferritin >684 ng/mL
- Platelet count <181,000/μL
- AST >48 U/L
- Fibrinogen <360 mg/dL
Treatment Strategies for MAS
Early and aggressive treatment is essential to manage MAS and prevent fatal complications. Treatment approaches include:
1. Corticosteroids
- First-line therapy (high-dose methylprednisolone or dexamethasone)
- Controls cytokine storm and inflammation
2. Immunomodulatory and Biologic Therapies
- IL-1 Inhibitors: Anakinra (rapid-acting and effective in sJIA-associated MAS)
- IL-6 Inhibitors: Tocilizumab (for cases resistant to IL-1 blockade)
- JAK Inhibitors: Ruxolitinib (emerging treatment for refractory MAS)
- TNF-α Inhibitors: Infliximab (less commonly used)
3. Cyclosporine A
- Calcineurin inhibitor that suppresses T-cell activation
- Often used in refractory MAS cases
4. Intravenous Immunoglobulin (IVIG)
- Immunomodulatory effects help regulate the immune system
- Beneficial in MAS triggered by infections
5. Etoposide (VP-16)
- Chemotherapy agent used in severe, refractory cases
- Part of HLH-94 and HLH-2004 treatment protocols
6. Supportive Care
- Plasmapheresis: Removes inflammatory cytokines in severe cases
- Anticoagulation Therapy: To manage disseminated intravascular coagulation (DIC)
- Organ Support: Ventilator support in ARDS cases, dialysis for renal failure
Prognosis and Long-Term Management
MAS has a high mortality rate if untreated, but early intervention improves outcomes. Key considerations for long-term management include:
- Regular monitoring of inflammatory markers (ferritin, cytokines, liver enzymes)
- Gradual tapering of immunosuppressive therapy to prevent relapses
- Lifestyle modifications to strengthen immune function and reduce infections
- Patient education on recognizing early MAS symptoms for prompt treatment