Chronic granulomatous disease (CGD) is a rare, inherited immunodeficiency disorder characterized by the inability of certain white blood cells to effectively kill certain types of bacteria and fungi. This defect leads to recurrent infections and the formation of granulomas—clusters of immune cells that develop as the body attempts to isolate and fight infections.
Understanding Chronic Granulomatous Disease
Causes and Genetic Basis
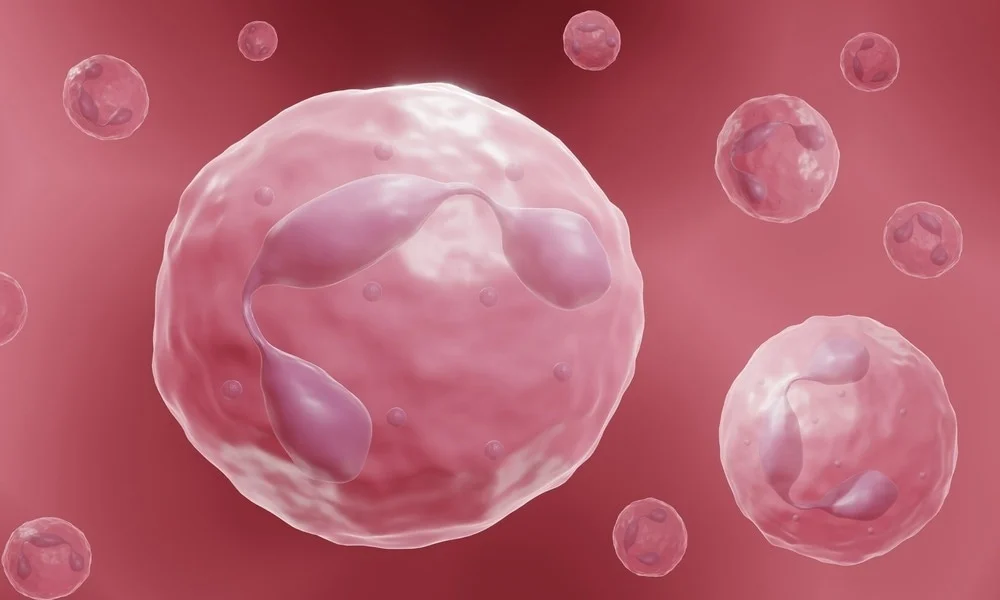
CGD results from mutations in genes responsible for the production of nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, a key enzyme in the oxidative burst of phagocytes. These mutations impair the ability of phagocytes, such as neutrophils and macrophages, to produce reactive oxygen species (ROS) necessary for killing pathogens.
CGD can be inherited in two primary ways:
- X-linked CGD: The most common form, caused by mutations in the CYBB gene on the X chromosome.
- Autosomal recessive CGD: Caused by mutations in other genes such as NCF1, NCF2, NCF4, or CYBA.
Epidemiology
CGD affects approximately 1 in 200,000 to 250,000 individuals worldwide. Males are predominantly affected due to the higher prevalence of X-linked CGD.
Symptoms
Patients with CGD typically present with:
- Recurrent bacterial and fungal infections, including pneumonia, abscesses, and osteomyelitis
- Granuloma formation, leading to obstruction in organs such as the gastrointestinal or urinary tract
- Delayed wound healing
- Chronic inflammation
Diagnosis
Laboratory Tests
Diagnosis of CGD involves specialized laboratory tests, including:
- Nitroblue Tetrazolium (NBT) Test: Measures the ability of neutrophils to produce ROS.
- Dihydrorhodamine 123 (DHR) Assay: A flow cytometry-based test that quantifies oxidative burst activity in phagocytes.
- Genetic Testing: Identifies mutations in NADPH oxidase-related genes.
Differential Diagnosis
Conditions such as leukocyte adhesion deficiency, hyper-IgE syndrome, and common variable immunodeficiency should be ruled out during diagnosis.
Treatment Options
Antibiotics and Antifungals
Prophylactic use of broad-spectrum antibiotics (e.g., trimethoprim-sulfamethoxazole) and antifungals (e.g., itraconazole) reduces the frequency and severity of infections.
Immunomodulation
Interferon-gamma (IFN-γ) therapy is used to enhance the immune response in CGD patients, though its efficacy may vary.
Hematopoietic Stem Cell Transplantation (HSCT)
HSCT is the only curative treatment for CGD. It involves replacing defective hematopoietic stem cells with healthy donor cells, typically from a matched sibling or unrelated donor.
Gene Therapy
Emerging gene therapy techniques aim to correct the genetic defect in patients with CGD. While promising, these approaches remain under investigation in clinical trials.
Management and Prognosis
Lifestyle Modifications
- Infection Prevention: Avoid exposure to high-risk environments such as soil, mulch, or unfiltered water.
- Hygiene: Maintain rigorous personal hygiene practices.
Monitoring
Regular follow-ups with an immunologist are essential to monitor infection risk and manage complications effectively.
Prognosis
With early diagnosis and appropriate management, many individuals with CGD can achieve improved quality of life. However, life expectancy may still be reduced compared to the general population, especially without access to advanced treatments.