Chronic Escherichia coli prostatitis, a persistent bacterial infection of the prostate gland, represents a significant urological concern. Characterized by recurrent urinary tract infections (UTIs) and chronic pelvic pain, it primarily affects men and can severely impact quality of life. In this article, we delve into the symptoms, causes, diagnostic methods, treatment options, and preventive measures for managing chronic E. coli prostatitis.
Understanding Chronic Escherichia Coli Prostatitis
Chronic prostatitis caused by E. coli bacteria is a form of chronic bacterial prostatitis (CBP). This condition occurs when E. coli bacteria colonize the prostate gland, leading to inflammation and recurrent infections. The infection can persist for weeks or months, often requiring targeted medical intervention.
Symptoms of Chronic E. Coli Prostatitis
Men with chronic E. coli prostatitis may experience the following symptoms:
- Urinary symptoms: Frequent urination, urgency, painful urination (dysuria), and difficulty emptying the bladder completely.
- Pelvic pain: Persistent discomfort or pain in the perineum, lower abdomen, or lower back.
- Sexual dysfunction: Pain during ejaculation and reduced libido.
- Systemic symptoms: Fatigue and mild fever during flare-ups.
The symptoms can vary in intensity and often overlap with other urological conditions, complicating the diagnosis.
Causes and Risk Factors
Primary Cause: E. Coli Bacteria
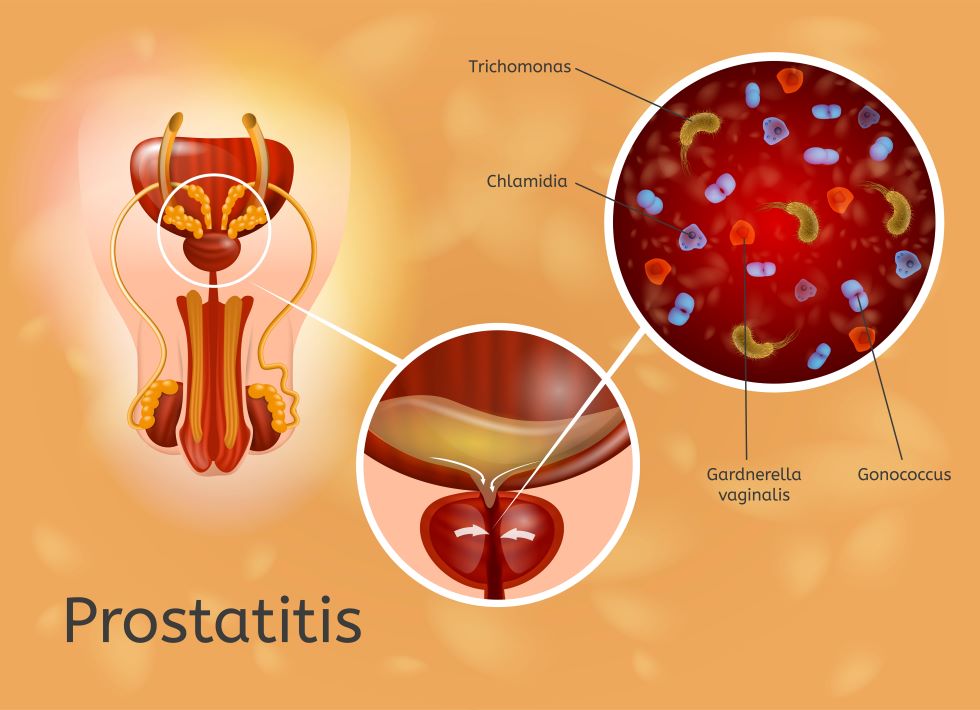
Escherichia coli, a common gram-negative bacterium, is the leading pathogen associated with chronic bacterial prostatitis. It can ascend from the urinary tract into the prostate gland, triggering infection.
Risk Factors
Several factors increase the risk of developing chronic E. coli prostatitis:
- Recurrent UTIs: Frequent urinary tract infections provide a reservoir for bacteria.
- Catheter use: Indwelling catheters can introduce bacteria into the urinary system.
- Prostate enlargement: Conditions like benign prostatic hyperplasia (BPH) can predispose individuals to prostatitis.
- Weakened immunity: Chronic illnesses or immunosuppressive therapy may contribute.
Diagnostic Approach
Accurate diagnosis is critical for effective treatment. Physicians typically employ the following methods:
Patient History and Symptom Assessment
A detailed medical history and symptom analysis help identify recurring patterns of infection and associated discomfort.
Laboratory Testing
- Urinalysis and urine culture: These tests confirm the presence of E. coli bacteria and rule out other pathogens.
- Semen culture: In some cases, semen analysis may be required.
Imaging Techniques
- Ultrasound: Transrectal ultrasound (TRUS) may identify prostate abnormalities.
- MRI: Used for complex cases to evaluate prostate structure in detail.
Treatment Options
Antibiotic Therapy
Long-term antibiotic treatment is the cornerstone of managing chronic E. coli prostatitis. Commonly prescribed antibiotics include:
- Fluoroquinolones: Ciprofloxacin and levofloxacin are effective against E. coli.
- Trimethoprim-sulfamethoxazole (TMP-SMX): A viable alternative for some patients.
Adjunct Therapies
- Alpha-blockers: These medications relax the muscles around the prostate, improving urinary flow.
- Anti-inflammatory agents: NSAIDs may help alleviate pain and inflammation.
Lifestyle Modifications
- Hydration: Adequate fluid intake helps flush bacteria from the urinary tract.
- Dietary changes: Avoiding irritants like caffeine and spicy foods can reduce symptoms.
Surgical Interventions
In rare cases, surgical procedures such as transurethral resection of the prostate (TURP) may be necessary to address structural issues.
Prevention Strategies
Good Hygiene Practices
Maintaining proper genital hygiene can reduce bacterial colonization and prevent infections.
Regular Medical Checkups
Routine urological evaluations help detect early signs of prostate issues.
Proactive Management of UTIs
Prompt treatment of urinary tract infections minimizes the risk of recurrence.
Strengthening Immunity
A balanced diet, regular exercise, and stress management bolster the immune system.