Chronic prostatitis is a complex condition that can significantly impact a patient’s quality of life. Among the various causes of prostatitis, Enterococcus faecalis stands out as a prominent and often difficult-to-treat bacterium responsible for chronic prostate infections. This article provides a comprehensive overview of chronic Enterococcus faecalis prostatitis, including its symptoms, diagnosis, and effective treatment options, while also offering insights into prevention and long-term management strategies.
What is Chronic Enterococcus faecalis Prostatitis?
Chronic prostatitis is a term used to describe persistent inflammation of the prostate gland that lasts for more than three months. Enterococcus faecalis, a Gram-positive bacterium, is one of the leading causes of bacterial prostatitis. This bacterium can persist within the prostate tissue, leading to ongoing symptoms and challenges in treatment.
While Enterococcus faecalis is generally considered a common microorganism found in the human gastrointestinal and urinary tracts, it can also cause infections in other body systems, including the prostate. The condition can present as chronic pelvic pain syndrome (CPPS) or bacterial prostatitis, both of which are marked by discomfort and potential long-term complications.
Symptoms of Chronic Enterococcus faecalis Prostatitis
The symptoms of chronic Enterococcus faecalis prostatitis can vary, but they are typically long-lasting and can affect several aspects of daily life. Common symptoms include:
- Pelvic pain: Persistent discomfort in the pelvic area, lower abdomen, and perineum.
- Painful urination: A burning sensation during urination is common.
- Frequent urination: Increased urgency to urinate, particularly at night (nocturia).
- Painful ejaculation: Discomfort during or after sexual activity.
- Reduced libido: Chronic discomfort can impact sexual drive and function.
- Lower back pain: Pain may radiate to the lower back, often exacerbated by prolonged sitting or physical activity.
Patients often experience a gradual onset of symptoms, which may flare up periodically, leading to periods of remission and exacerbation.
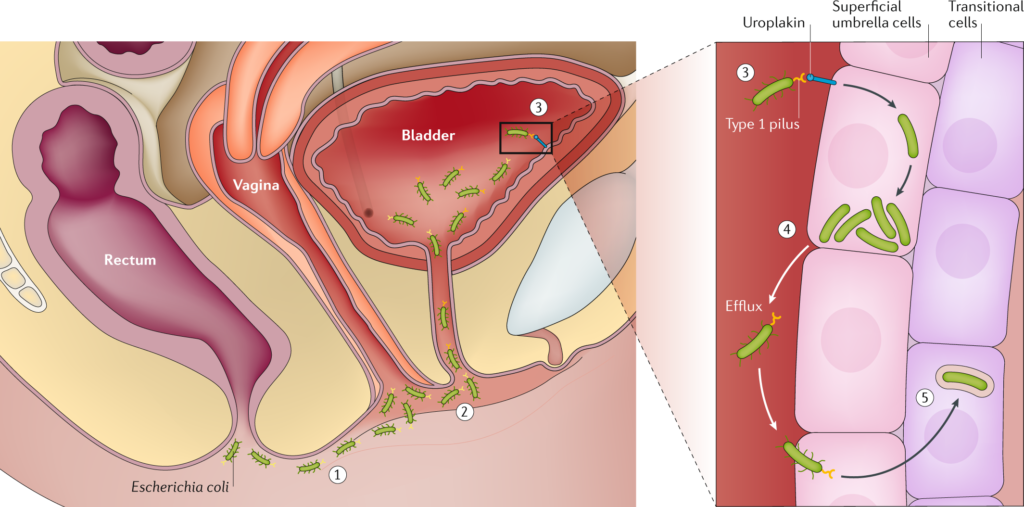
How Enterococcus faecalis Causes Prostatitis
Enterococcus faecalis can enter the prostate through the urethra, often during an infection in the urinary tract. Once in the prostate, the bacterium can evade the immune system, potentially leading to chronic infection. It thrives in the prostate’s unique environment, where it can form biofilms that protect it from antibiotics and immune defenses. This biofilm formation is one of the primary reasons chronic Enterococcus faecalis prostatitis is so difficult to treat.
The bacteria may also trigger an immune response that exacerbates inflammation, leading to further pain and discomfort. Due to its resistance to certain antibiotics and the potential for biofilm-related persistence, treatment can be prolonged and require specialized approaches.
Diagnosis of Chronic Enterococcus faecalis Prostatitis
Accurate diagnosis is essential for effectively managing chronic Enterococcus faecalis prostatitis. Healthcare providers typically employ several diagnostic methods:
1. Medical History and Symptom Review
A thorough evaluation of the patient’s medical history, including any previous urinary tract infections (UTIs) or prostatitis episodes, is critical. Symptom assessment, including pelvic pain and urination difficulties, helps guide the diagnostic process.
2. Physical Examination
A digital rectal examination (DRE) is performed to evaluate prostate size, tenderness, and possible abnormalities. Tenderness or swelling in the prostate area may indicate inflammation or infection.
3. Urine and Prostate Secretions Culture
A key diagnostic tool is culturing urine or prostate fluid to identify the presence of Enterococcus faecalis. This is typically done by collecting expressed prostatic secretion (EPS) or midstream urine samples, followed by microbiological analysis. If Enterococcus faecalis is found in high numbers, a diagnosis of bacterial prostatitis can be confirmed.
4. PSA Test
Prostate-specific antigen (PSA) levels may be elevated during prostatitis, although this test alone cannot diagnose chronic prostatitis. However, it can help rule out other conditions, such as prostate cancer.
5. Transrectal Ultrasound
In some cases, imaging such as transrectal ultrasound may be utilized to assess the prostate’s structure and identify any abscesses or abnormalities that might be contributing to the symptoms.
Treatment Options for Chronic Enterococcus faecalis Prostatitis
Effective treatment of chronic Enterococcus faecalis prostatitis requires a multifaceted approach, typically including antibiotics, anti-inflammatory medications, and sometimes lifestyle changes. The goal of treatment is to reduce inflammation, control infection, and manage symptoms.
1. Antibiotic Therapy
The cornerstone of treatment is the use of antibiotics. Since Enterococcus faecalis is often resistant to some common antibiotics, the choice of drug is crucial. Common antibiotics used for treatment include:
- Fluoroquinolones: Ciprofloxacin and levofloxacin are often effective against Enterococcus faecalis.
- Trimethoprim-sulfamethoxazole: This combination can also target Enterococcus faecalis.
- Penicillin-based antibiotics: These can be prescribed if the strain is susceptible.
Treatment duration is typically longer than for other types of prostatitis, often lasting 4 to 6 weeks, due to the difficulty in eradicating the infection and the tendency for biofilm formation.
2. Alpha-blockers
Alpha-blockers, such as tamsulosin, can help reduce symptoms of urinary urgency and frequency by relaxing the muscles of the bladder and prostate.
3. Anti-inflammatory Medications
Non-steroidal anti-inflammatory drugs (NSAIDs) or corticosteroids may be prescribed to reduce inflammation and relieve pain associated with prostatitis.
4. Lifestyle Modifications
Patients are encouraged to make certain lifestyle changes to support the healing process, including:
- Increasing fluid intake to help flush out bacteria from the urinary tract.
- Avoiding caffeine and alcohol, which can irritate the bladder and prostate.
- Regular pelvic floor exercises to improve prostate function and reduce pain.
5. Surgical Intervention
In rare cases, surgical procedures may be necessary if abscesses or other complications arise. Surgery may also be considered if the infection is refractory to antibiotics or other treatments.
Preventing Chronic Enterococcus faecalis Prostatitis
While complete prevention of chronic Enterococcus faecalis prostatitis may not always be possible, certain steps can reduce the risk of infection:
- Proper hygiene practices: Maintaining good personal hygiene, especially during sexual activity, can help prevent the introduction of bacteria into the urinary tract and prostate.
- Regular medical check-ups: Early diagnosis and treatment of any urinary tract infections can prevent the spread of bacteria to the prostate.
- Prompt treatment of UTIs: Addressing urinary tract infections promptly can reduce the risk of these infections ascending to the prostate.
Long-Term Management and Outlook
Chronic prostatitis can be a long-term condition that requires ongoing management. Most patients benefit from a combination of medical treatment and lifestyle adjustments. Although some individuals may experience periodic flare-ups, many find significant relief through targeted therapy. However, a small percentage of patients may experience persistent symptoms despite treatment, requiring additional medical interventions.
By understanding the nature of chronic Enterococcus faecalis prostatitis and implementing appropriate diagnostic and therapeutic strategies, healthcare providers can offer patients the best chance at managing this challenging condition.