Chlamydial epididymitis refers to the inflammation of the epididymis caused by an infection with Chlamydia trachomatis. The condition is often associated with sexually transmitted infections (STIs) and primarily affects sexually active males. This article delves into the causes, symptoms, diagnostic methods, treatment options, and prevention strategies for chlamydial epididymitis.
Understanding the Epididymis
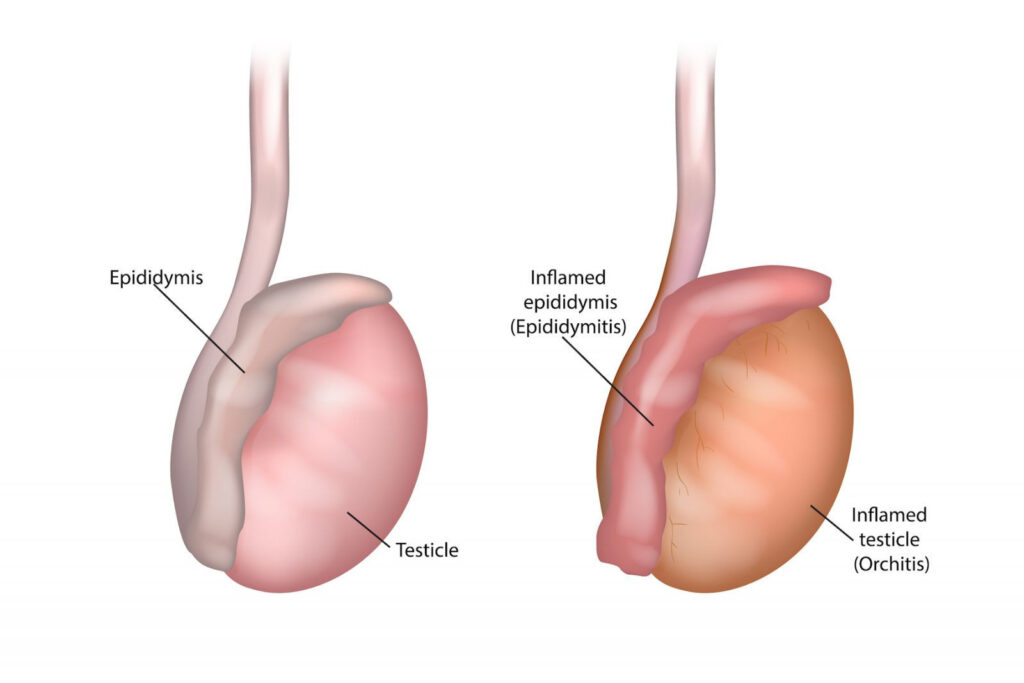
The epididymis is a coiled tube located at the back of the testicle, responsible for storing and transporting sperm. Infections, particularly those caused by Chlamydia trachomatis, can lead to inflammation, causing discomfort and potential complications if left untreated.
Causes of Chlamydial Epididymitis
Chlamydial epididymitis primarily results from the spread of Chlamydia trachomatis through sexual contact. The following factors can increase the risk of developing this condition:
- Unprotected sexual activity
- Multiple sexual partners
- Previous history of sexually transmitted infections
- Anatomical abnormalities of the urinary tract
Other pathogens, such as Neisseria gonorrhoeae, can also co-infect and contribute to epididymitis.
Symptoms
Symptoms of chlamydial epididymitis can range from mild to severe and typically develop over several days. Common signs include:
- Scrotal pain and tenderness
- Swelling and redness of the scrotum
- Painful urination (dysuria)
- Discharge from the penis
- Fever and chills in more severe cases
- Testicular discomfort, sometimes radiating to the groin
If left untreated, complications such as infertility, chronic pain, or abscess formation may arise.
Diagnosis
Diagnosing chlamydial epididymitis involves a combination of clinical evaluation and laboratory tests. The following methods are commonly used:
- Medical History and Physical Examination
- Assessment of sexual history
- Palpation of the scrotum to detect swelling and tenderness
- Laboratory Tests
- Urine Tests: To identify the presence of C. trachomatis or other pathogens.
- Urethral Swab: Used for collecting samples to detect sexually transmitted infections.
- Imaging
- Ultrasound: To rule out other conditions like testicular torsion and confirm epididymal inflammation.
Treatment
Treatment for chlamydial epididymitis focuses on eliminating the infection and managing symptoms. Key treatment approaches include:
Antibiotic Therapy
- First-line Antibiotics:
- Doxycycline (100 mg twice daily for 10-14 days)
- Azithromycin (1 g single dose, though less commonly used for epididymitis)
- In cases of co-infection with Neisseria gonorrhoeae, ceftriaxone may be added.
Symptomatic Management
- Analgesics (e.g., ibuprofen) for pain relief
- Scrotal elevation and cold packs to reduce swelling
- Adequate hydration and rest
Partner Notification and Treatment
To prevent reinfection, sexual partners should be tested and treated for chlamydia.
Prevention
Preventing chlamydial epididymitis involves reducing the risk of chlamydial infections. Key preventive measures include:
- Consistent and correct use of condoms
- Regular STI screenings for sexually active individuals
- Limiting the number of sexual partners
- Prompt treatment of any diagnosed sexually transmitted infections
Potential Complications
If left untreated, chlamydial epididymitis may lead to:
- Chronic epididymal pain
- Infertility due to damage to the reproductive tract
- Abscess formation
- Dissemination of the infection to other areas, such as the testes (epididymo-orchitis)

