Chemotherapy-induced anemia is a common complication faced by cancer patients undergoing chemotherapy. It significantly impacts quality of life and can compromise treatment outcomes if left untreated. This article delves into its causes, symptoms, treatment options, and effective management strategies.
What Is Chemotherapy-Induced Anemia?
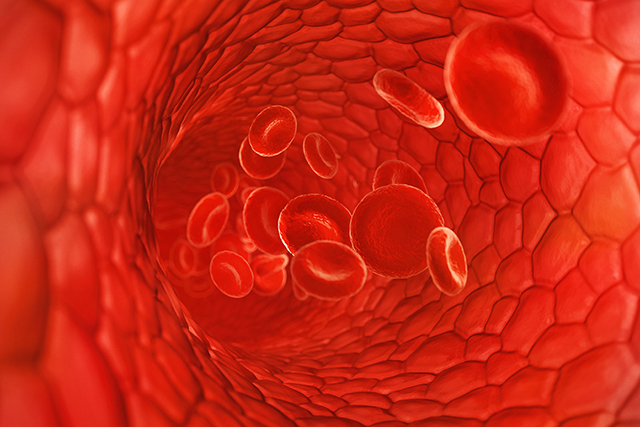
Anemia is a condition characterized by a decrease in the number of red blood cells (RBCs) or hemoglobin levels, leading to reduced oxygen-carrying capacity of the blood. In the context of chemotherapy, this type of anemia is primarily caused by the myelosuppressive effects of cancer treatments, which interfere with bone marrow’s ability to produce RBCs.
Causes of Chemotherapy-Induced Anemia
- Bone Marrow Suppression: Chemotherapy drugs target rapidly dividing cells, including those in the bone marrow, reducing RBC production.
- Nutritional Deficiencies: Treatments can impair appetite, leading to deficiencies in iron, vitamin B12, and folic acid.
- Inflammatory Cytokines: Cancer and chemotherapy stimulate the production of cytokines that can suppress erythropoiesis.
- Blood Loss: Tumor-associated bleeding or invasive procedures can contribute to anemia.
Recognizing Symptoms of Anemia
Patients with chemotherapy-induced anemia may experience symptoms such as:
- Persistent fatigue and weakness
- Shortness of breath
- Dizziness or lightheadedness
- Pale skin or pallor
- Rapid heartbeat
- Reduced exercise tolerance
These symptoms may vary in severity and often overlap with those of cancer itself.
Diagnosis of Chemotherapy-Induced Anemia
Diagnosis involves:
- Complete Blood Count (CBC): Measures hemoglobin levels, hematocrit, and RBC count.
- Reticulocyte Count: Assesses bone marrow activity.
- Iron Studies: Evaluates serum ferritin, transferrin saturation, and total iron-binding capacity.
- Vitamin Levels: Checks for deficiencies in vitamin B12 and folic acid.
Treatment Options
1. Erythropoiesis-Stimulating Agents (ESAs)
ESAs, such as epoetin alfa and darbepoetin alfa, stimulate RBC production. While effective, their use requires monitoring due to potential risks, including thromboembolic events.
2. Iron Supplementation
- Oral Iron: Suitable for patients with mild anemia.
- Intravenous (IV) Iron: Recommended for those with significant iron deficiency or malabsorption issues.
3. Blood Transfusions
Transfusions provide immediate relief by increasing RBC count. However, they are typically reserved for severe cases due to risks like iron overload and alloimmunization.
4. Nutritional Support
Ensuring adequate intake of iron, vitamin B12, and folic acid through diet or supplements is crucial for anemia prevention and recovery.
Management Strategies
Monitoring and Early Detection
Regular blood tests during chemotherapy allow for early identification and intervention of anemia, minimizing complications.
Patient Education
Educating patients about anemia symptoms enables timely reporting and proactive management.
Multidisciplinary Approach
Collaboration between oncologists, hematologists, and dietitians ensures comprehensive care tailored to individual patient needs.
Prognosis and Quality of Life
Effective management of chemotherapy-induced anemia improves energy levels, physical functioning, and overall well-being. It also supports adherence to cancer treatment regimens, optimizing therapeutic outcomes.