Von Willebrand’s disease (vWD) is the most common inherited bleeding disorder, caused by a deficiency or dysfunction of von Willebrand factor (vWF), a crucial protein involved in blood clotting. Unlike hemophilia, which primarily affects males, vWD affects both genders equally and can vary in severity from mild to life-threatening.
Understanding the Role of von Willebrand Factor in Clotting
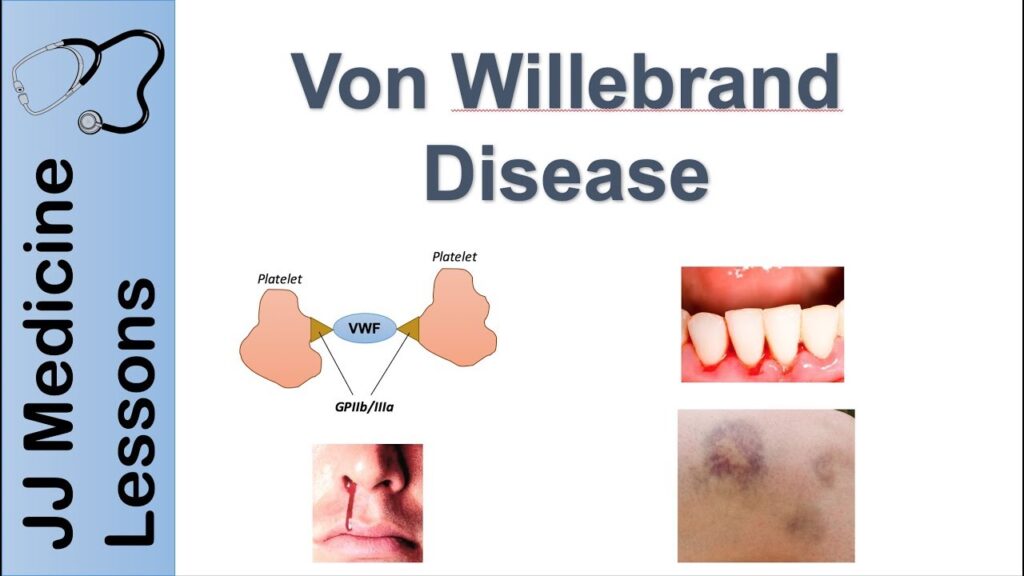
Von Willebrand factor plays a dual role in hemostasis: it helps platelets stick to the damaged endothelium and stabilizes factor VIII, another essential clotting protein. A deficiency or abnormality in vWF disrupts this process, resulting in prolonged bleeding.
Types of Von Willebrand’s Disease
vWD is classified into three primary types based on quantitative and qualitative deficiencies of vWF.
Type 1: Partial Quantitative Deficiency
- Most common (approximately 75% of cases)
- Reduced levels of normal vWF
- Symptoms usually mild
- Inherited in an autosomal dominant manner
Type 2: Qualitative Deficiency
- Normal vWF quantity but abnormal function
- Subtypes include:
- 2A: Lack of high-molecular-weight vWF multimers
- 2B: Increased platelet binding leading to removal of vWF
- 2M: Defective platelet binding, but normal multimer distribution
- 2N: Impaired binding to factor VIII (resembles hemophilia A)
Type 3: Total Deficiency
- Rare and most severe form
- Very low or absent vWF levels
- Inherited in an autosomal recessive pattern
- Often associated with severe mucocutaneous and joint bleeding
Symptoms and Clinical Manifestations of vWD
Bleeding tendencies vary based on the type and severity of the disease. Symptoms often emerge during childhood or adolescence and may worsen during menstruation, surgery, or trauma.
Common Symptoms:
- Frequent nosebleeds (epistaxis)
- Easy bruising
- Prolonged bleeding from cuts or dental work
- Heavy or prolonged menstrual bleeding (menorrhagia)
- Blood in urine or stool
- Excessive bleeding after childbirth or surgery
- Joint and muscle bleeds (more common in Type 3)
Diagnosing Von Willebrand’s Disease
Early and accurate diagnosis is critical for effective management. It involves a thorough evaluation of personal and family bleeding history, physical examination, and laboratory tests.
Diagnostic Tests:
- vWF Antigen: Measures amount of vWF in blood
- Ristocetin Cofactor Activity (vWF:RCo): Assesses vWF function
- Factor VIII Activity: Evaluates associated clotting protein
- Multimer Analysis: Determines the structure of vWF
- Platelet Function Analyzer (PFA-100): Simulates clotting under flow conditions
- Genetic Testing: Used in complex or unclear cases
Inheritance Patterns and Genetic Basis
Von Willebrand’s disease is inherited, with different types following distinct genetic patterns.
- Type 1 and 2: One copy of the mutated gene can cause the disorder
- Type 3: Requires two mutated gene copies, one from each parent
Differential Diagnosis
It is essential to distinguish vWD from other bleeding disorders for targeted treatment.
- Hemophilia A/B: Primarily joint bleeding, X-linked inheritance
- Platelet function disorders: Normal vWF, but defective platelet aggregation
- Thrombocytopenia: Low platelet count rather than protein dysfunction
- Acquired vWD: Secondary to other conditions like hypothyroidism or autoimmune disorders
Treatment and Management Strategies
The goal of treatment is to prevent and control bleeding episodes. Therapy depends on disease type, severity, and patient needs.
1. Desmopressin (DDAVP)
- Stimulates release of stored vWF and factor VIII
- Effective in Type 1 and some Type 2 cases
- Administered intranasally or intravenously
- Not suitable for Type 3
2. vWF-Containing Factor Concentrates
- For patients unresponsive to DDAVP or with Type 3
- Plasma-derived or recombinant products
- Used during surgery, trauma, or severe bleeding episodes
3. Antifibrinolytic Agents
- e.g., Tranexamic acid or aminocaproic acid
- Useful in mucosal bleeding and dental procedures
- Often used in combination with other therapies
4. Hormonal Therapy
- Oral contraceptives can help manage heavy menstrual bleeding
- Levonorgestrel-releasing intrauterine devices (IUDs) also effective
5. Supportive Measures
- Avoid NSAIDs and aspirin
- Use caution during dental or surgical procedures
- Consider hematologist consultation for individualized care plans
Living with Von Willebrand’s Disease
Lifestyle and Precautionary Measures:
- Wear a medical alert bracelet
- Inform healthcare providers before surgery or dental work
- Maintain oral hygiene to avoid gum bleeding
- Use protective gear during sports or physical activity
- Regular checkups with a hematologist
Special Considerations: Women and vWD
Women with vWD face unique challenges, particularly related to menstruation, childbirth, and miscarriage.
Key Issues:
- Menorrhagia is often the first sign of vWD in females
- Postpartum hemorrhage risk is significantly higher
- Obstetricians must be involved in delivery planning
- Hormonal treatments can effectively manage symptoms
Complications Associated with vWD
- Anemia from chronic blood loss
- Post-surgical hemorrhage
- Joint damage from repeated bleeds (in severe cases)
- Psychosocial impact due to activity restrictions and anxiety
Future Directions in vWD Management
- Development of long-acting vWF products
- Gene therapy research for potential permanent correction
- Enhanced diagnostic tools for precise subtype identification
- Patient registries to improve data collection and treatment outcomes
Von Willebrand’s disease, while often underdiagnosed, represents a significant cause of bleeding disorders worldwide. Accurate diagnosis, appropriate treatment tailored to the type and severity, and patient education are essential for optimal management. With ongoing research and advancements in therapy, outcomes for patients with vWD continue to improve, offering a better quality of life and reduced risk of serious complications.

