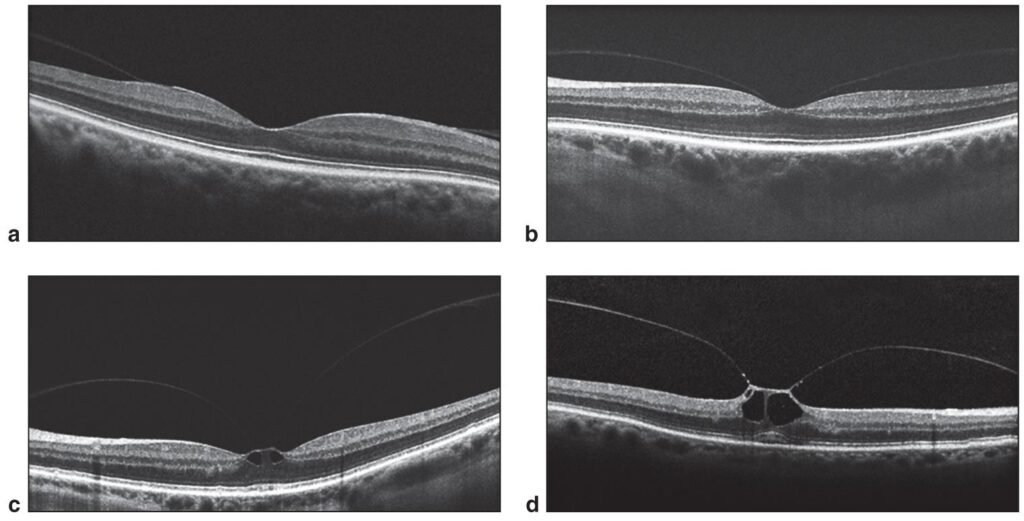
Vitreomacular adhesion (VMA) is a pathological condition where the vitreous gel adheres abnormally to the macula, the central part of the retina responsible for sharp, central vision. While posterior vitreous detachment (PVD) is a natural part of aging, incomplete separation at the macula can lead to persistent traction and anatomical distortion, which may compromise visual function.
Anatomy and Pathophysiology of the Vitreomacular Interface
The posterior vitreous cortex is normally attached to the retina at several points, including the macula. With age, liquefaction of the vitreous body (synchysis) and weakening of the vitreoretinal interface occur. However, if vitreous liquefaction outpaces detachment from the retina, the residual adhesion at the macula creates persistent traction.
Key Concepts:
- Physiological PVD: Complete separation of vitreous from the retina
- Pathologic VMA: Partial separation with persistent macular adhesion
- Vitreomacular Traction (VMT): When VMA exerts anteroposterior traction, causing visual distortion and potential structural damage
Classification of VMA and VMT
The International Vitreomacular Traction Study (IVTS) Group classifies VMA based on size and association with retinal pathology.
Classification Criteria:
- Focal VMA: ≤ 1500 µm adhesion area
- Broad VMA: > 1500 µm adhesion area
- VMA with VMT: Associated with retinal distortion (macular hole, edema, or tractional detachment)
Symptoms and Clinical Presentation
VMA may be asymptomatic or present with visual disturbances when traction affects retinal integrity.
Common Symptoms:
- Metamorphopsia (distorted vision)
- Blurred or decreased central vision
- Micropsia or macropsia (size distortion)
- Photopsia (flashes of light)
Symptom severity often correlates with the extent of traction rather than the size of adhesion.
Diagnostic Techniques for VMA
Accurate diagnosis relies on multimodal imaging, particularly spectral-domain optical coherence tomography (SD-OCT), which provides high-resolution cross-sectional views of the macula.
Diagnostic Modalities:
- OCT Imaging: Essential for identifying VMA, VMT, and associated macular changes
- Fundus Photography: Useful for documenting baseline retinal structure
- Fluorescein Angiography: May show macular edema or leakage
- Ultrasound B-scan: Used in cases with media opacities
Natural History and Prognosis of Vitreomacular Adhesion
Spontaneous resolution of VMA occurs in a subset of patients, particularly in cases with focal adhesion. However, persistent VMA can progress to vision-threatening complications.
Possible Outcomes:
- Spontaneous Posterior Vitreous Detachment
- Progression to VMT or Macular Hole
- Development of Cystoid Macular Edema (CME)
- Chronic Traction and Photoreceptor Damage
Monitoring progression is crucial, with intervention considered when functional vision is compromised.
Therapeutic Strategies for Vitreomacular Adhesion
Management of VMA ranges from observation in asymptomatic patients to pharmacologic or surgical intervention in symptomatic cases.
1. Observation and Monitoring
- Appropriate for asymptomatic or mild cases
- Regular OCT follow-up to detect changes
- Patient education on symptom progression
2. Pharmacologic Vitreolysis (Ocriplasmin)
Ocriplasmin is a recombinant protease approved for the treatment of symptomatic VMA and small macular holes.
Mechanism of Action:
- Enzymatic cleavage of fibronectin and laminin at the vitreoretinal interface
- Facilitates vitreous detachment and adhesion release
Indications:
- Focal VMA without epiretinal membrane
- VMA associated with small full-thickness macular hole (<400 µm)
- No significant lens pathology (due to photopsia risk)
Efficacy:
- VMA resolution in ~26% of cases after single injection
- Best outcomes with early intervention and careful patient selection
3. Pars Plana Vitrectomy (PPV)
Surgical intervention remains the definitive treatment in severe or refractory VMA and traction cases.
Indications:
- Persistent VMT with significant visual symptoms
- Failed pharmacologic therapy
- Macular hole formation or progression
- Coexisting retinal pathologies (e.g., epiretinal membrane, diabetic macular edema)
Procedure:
- Removal of vitreous gel and release of adhesion
- Often combined with ILM peeling to reduce recurrence
- Use of vital dyes (e.g., triamcinolone, BBG) for enhanced visualization
Comparative Overview of Treatment Approaches
| Treatment Modality | Indicated For | Advantages | Limitations |
|---|---|---|---|
| Observation | Asymptomatic or mild VMA | Non-invasive, no risk | Requires close follow-up |
| Ocriplasmin Injection | Focal VMA, small macular holes | Minimally invasive, outpatient | Variable response, potential side effects |
| Vitrectomy | Symptomatic VMT, large adhesions | High success rate, customizable | Surgical risks, recovery period |
Emerging Therapies and Future Directions
Research is ongoing into safer, more effective pharmacologic agents and less invasive surgical techniques.
Innovations in Development:
- Second-generation proteolytics with higher efficacy
- Biodegradable vitreolytic implants for sustained release
- iOCT-assisted vitrectomy for real-time traction assessment
- AI-driven OCT analytics for earlier detection and prognosis modeling
These advancements aim to expand treatment access and precision for patients with VMA.
Vitreomacular adhesion is a significant pathology affecting the macula that may lead to vision impairment if left untreated. Early identification using OCT and appropriate classification guide treatment decisions. While many cases resolve spontaneously, pharmacologic vitreolysis and vitrectomy offer effective solutions for symptomatic or progressing VMA. Ongoing innovations in imaging and therapeutics promise further refinement in managing this complex condition.