Vitiligo is a long-term dermatological condition characterized by the progressive loss of skin pigmentation, resulting in white patches due to the destruction or dysfunction of melanocytes—the cells responsible for melanin production. This condition can affect any part of the body and occurs across all skin types, although it is more noticeable in individuals with darker skin. Vitiligo is not contagious or life-threatening but may lead to psychological distress and social stigma.

Causes of Vitiligo: Exploring the Underlying Mechanisms
While the exact cause remains unclear, vitiligo is widely believed to result from a complex interplay of genetic, autoimmune, oxidative stress, and neurogenic factors.
1. Autoimmune Response
The immune system mistakenly targets and destroys melanocytes. This theory is supported by the frequent co-occurrence of vitiligo with other autoimmune diseases such as Hashimoto’s thyroiditis, alopecia areata, and type 1 diabetes.
2. Genetic Predisposition
Up to 30% of vitiligo patients report a family history. Several genes, including NLRP1, PTPN22, and TYR, have been associated with susceptibility.
3. Oxidative Stress
An imbalance between free radicals and antioxidants in the skin may damage melanocytes, leading to pigment loss.
4. Neurogenic Factors
Certain neurochemicals may be toxic to melanocytes, particularly in segmental vitiligo.
Types of Vitiligo: Classification by Distribution and Pattern
Vitiligo is categorized based on the pattern and extent of depigmentation.
1. Non-Segmental Vitiligo (NSV)
The most common form, characterized by bilateral and symmetrical white patches. Subtypes include:
- Generalized Vitiligo: Wide body distribution
- Acrofacial Vitiligo: Affecting face, hands, and feet
- Mucosal Vitiligo: Involving mucous membranes
2. Segmental Vitiligo (SV)
Presents unilaterally in a localized area, often along a dermatome. It typically has an early onset and rapid progression that stabilizes over time.
3. Mixed Vitiligo
Features both segmental and non-segmental characteristics.
4. Universal Vitiligo
Extensive depigmentation over most of the body’s surface.
Symptoms and Clinical Features
Vitiligo’s hallmark symptom is the appearance of flat, depigmented patches of skin. Key features include:
- Irregular or well-defined white macules
- Symmetrical distribution (in NSV)
- Premature graying of hair (scalp, eyebrows, eyelashes)
- Mucosal involvement (oral, genital areas)
- Sun sensitivity in affected areas
Vitiligo does not usually cause physical discomfort, but the psychological impact can be profound, especially in visible areas.
Diagnostic Evaluation of Vitiligo
Diagnosis is primarily clinical, but further investigations can confirm and rule out differential diagnoses.
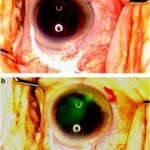
1. Wood’s Lamp Examination
Highlights depigmented areas with a blue-white fluorescence.
2. Skin Biopsy
May reveal absence of melanocytes and perivascular lymphocytic infiltration.
3. Blood Tests
Used to screen for associated autoimmune conditions:
- Thyroid function tests
- ANA (antinuclear antibodies)
- Vitamin B12 and folate levels
Treatment Options for Vitiligo
While there is no definitive cure, multiple treatment modalities aim to halt progression, repigment the skin, and improve cosmetic appearance.
1. Topical Therapies
- Corticosteroids: Effective in localized cases, especially early stages
- Calcineurin Inhibitors (Tacrolimus, Pimecrolimus): Preferred for facial and intertriginous areas
- Vitamin D analogs: Sometimes combined with corticosteroids
2. Phototherapy
- Narrowband UVB (NB-UVB): Standard for widespread vitiligo
- PUVA (Psoralen + UVA): Less commonly used due to higher side-effect profile
3. Surgical Treatments
Considered for stable vitiligo when medical therapies fail:
- Punch grafting
- Blister grafting
- Cell suspension transplantation
4. Depigmentation Therapy
For extensive cases, the remaining pigmented skin can be depigmented with monobenzyl ether of hydroquinone to achieve a uniform appearance.
5. Camouflage and Cosmetic Solutions
- Medical-grade camouflage makeup
- Self-tanning products
- Micropigmentation (tattooing)
6. Emerging Therapies
- Janus Kinase (JAK) inhibitors (e.g., tofacitinib, ruxolitinib) show promising early results
- Afamelanotide (a melanocyte-stimulating analog) under research
- Platelet-Rich Plasma (PRP) Therapy being studied for regenerative effects
Disease Course and Prognosis
Vitiligo is unpredictable in progression. Some patients may experience spontaneous repigmentation, particularly in sun-exposed areas, while others observe continual depigmentation. Segmental vitiligo tends to stabilize earlier than non-segmental types. Early intervention can significantly improve treatment outcomes.
Living With Vitiligo: Coping and Support
Psychosocial impact should not be underestimated. Patients may face emotional distress, social withdrawal, and self-esteem issues. Counseling, support groups, and public education play a vital role in promoting acceptance and reducing stigma.
Prevention and Risk Reduction
While vitiligo cannot always be prevented, certain strategies may reduce triggers or slow its progression:
- Protecting skin from trauma and sunburn
- Managing stress levels
- Avoiding harsh chemical exposures
- Early treatment initiation upon diagnosis
Differential Diagnosis: Distinguishing Vitiligo from Other Disorders
| Condition | Key Differences |
|---|---|
| Tinea Versicolor | Scaling patches, fungal infection, positive KOH |
| Pityriasis Alba | Hypopigmented, not depigmented; mild scaling |
| Post-inflammatory hypopigmentation | History of trauma or inflammation |
| Albinism | Congenital absence of pigment, no acquired pattern |
| Chemical leukoderma | Contact history with bleaching agents |
Vitiligo is a chronic, often progressive skin disorder resulting in loss of pigmentation due to melanocyte destruction. Although its etiology is multifactorial—spanning autoimmune, genetic, and environmental components—it can be managed effectively through a combination of medical, surgical, and supportive therapies. With advancements in immunomodulatory treatments and repigmentation strategies, outcomes continue to improve. Emphasizing early diagnosis, patient education, and psychosocial support remains essential to holistic management.