Vitamin K deficiency-induced hypoprothrombinemia is a coagulopathy resulting from impaired synthesis of vitamin K-dependent clotting factors—primarily prothrombin (Factor II). This disorder is characterized by a marked prolongation of the prothrombin time (PT) and heightened bleeding risk. As vitamin K plays a critical role in the carboxylation of several clotting factors, any disruption in its availability or metabolism can lead to profound hemorrhagic manifestations.
The Essential Role of Vitamin K in Hemostasis
Vitamin K is integral to hepatic production of clotting factors II, VII, IX, and X, as well as proteins C and S. It facilitates γ-carboxylation of glutamic acid residues on these proteins, enabling calcium binding and proper activation.
In the absence of sufficient vitamin K, undercarboxylated and nonfunctional clotting proteins—termed PIVKA (Proteins Induced by Vitamin K Absence)—accumulate, impairing the coagulation cascade and predisposing individuals to bleeding.
Primary Causes of Vitamin K Deficiency-Induced Hypoprothrombinemia
1. Dietary Insufficiency
Although rare in adults, dietary vitamin K deficiency may occur in cases of:
- Poor nutritional intake
- Alcoholism
- Prolonged fasting
2. Fat Malabsorption Syndromes
Given vitamin K’s fat-soluble nature, any impairment in lipid absorption reduces its bioavailability. Common etiologies include:
- Cystic fibrosis
- Chronic pancreatitis
- Celiac disease
- Inflammatory bowel disease
- Biliary obstruction
3. Hepatobiliary Disorders
Liver dysfunction compromises both the storage of vitamin K and synthesis of clotting factors. Conditions such as:
- Cirrhosis
- Biliary atresia
- Primary sclerosing cholangitis
…are frequently associated with secondary hypoprothrombinemia.
4. Drug-Induced Hypoprothrombinemia
Several pharmacologic agents interfere with vitamin K metabolism or its dependent pathways:
- Warfarin (vitamin K antagonist)
- Cephalosporins with N-methylthiotetrazole (NMTT) side chains
- Broad-spectrum antibiotics (disrupt gut flora synthesizing vitamin K2)
- Salicylates and sulfonamides (affect hepatic enzyme function)
5. Neonatal Deficiency
Newborns are particularly vulnerable due to:
- Low hepatic stores of vitamin K
- Sterile intestines (limited bacterial synthesis)
- Inadequate placental transfer
This can lead to Vitamin K Deficiency Bleeding (VKDB) in neonates.
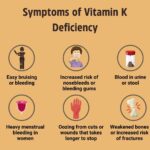
Clinical Manifestations of Hypoprothrombinemia
Symptoms emerge as the deficiency progresses and the clotting cascade becomes increasingly ineffective. These include:
- Easy bruising and mucosal bleeding
- Hematuria
- Gastrointestinal bleeding
- Intracranial hemorrhage (especially in neonates)
- Post-surgical or post-traumatic prolonged bleeding
The clinical severity often correlates with the degree of prothrombin time prolongation.
Diagnostic Workup
1. Prothrombin Time (PT)
- Most sensitive indicator of hypoprothrombinemia
- Prolonged PT with a normal aPTT in early stages
2. INR (International Normalized Ratio)
- Standardized PT used to monitor warfarin therapy and assess coagulopathy severity
3. Factor II Assay
- Direct measurement confirms reduced prothrombin levels
4. PIVKA-II Levels
- Elevated in cases of vitamin K deficiency
- Useful in distinguishing between vitamin K deficiency and liver disease
5. Liver Function Tests and Stool Fat Analysis
- Helps identify secondary causes like hepatic disease or fat malabsorption
Treatment of Vitamin K Deficiency-Induced Hypoprothrombinemia
1. Vitamin K Supplementation
Route and dosage depend on severity and underlying cause:
- Oral: 2.5–25 mg for mild deficiency
- Intramuscular or intravenous: 5–10 mg for severe or active bleeding
- Neonatal prophylaxis: 0.5–1 mg IM at birth
Note: IV administration should be given slowly to reduce the risk of anaphylactoid reactions.
2. Plasma or Prothrombin Complex Concentrates (PCC)
- For immediate reversal in bleeding emergencies or prior to surgery
- Useful in cases of warfarin toxicity with active hemorrhage
3. Management of Underlying Conditions
- Treat liver disease, restore bile flow, or address malabsorption
- Discontinue or adjust interfering medications
4. Antibiotic-Associated Hypoprothrombinemia
- Supplement with vitamin K if prolonged PT develops during prolonged antibiotic therapy
Prognosis and Prevention
When recognized early and treated appropriately, vitamin K deficiency-induced hypoprothrombinemia has an excellent prognosis. In neonates, universal prophylaxis has significantly reduced incidence and mortality from VKDB. In high-risk adult populations, especially those on warfarin or with malabsorption disorders, periodic monitoring of PT/INR and vitamin K supplementation are essential preventive strategies.
Differential Diagnosis
Distinguishing vitamin K deficiency-induced hypoprothrombinemia from other causes of bleeding disorders is critical:
| Condition | PT | aPTT | Platelet Count | Clotting Factors |
|---|---|---|---|---|
| Vitamin K Deficiency | ↑ | Normal | Normal | II, VII, IX, X ↓ |
| Liver Disease | ↑ | ↑ | Normal/↓ | All ↓ |
| DIC | ↑ | ↑ | ↓ | All ↓ |
| Hemophilia A/B | Normal | ↑ | Normal | VIII or IX ↓ |
Vitamin K deficiency-induced hypoprothrombinemia remains a clinically important, yet highly treatable condition that can lead to severe bleeding if unrecognized. Early detection through PT/INR testing and a clear understanding of etiologic factors—ranging from dietary deficits to drug interactions—ensures prompt intervention and improved outcomes. Prophylactic strategies, especially in neonates and at-risk adults, remain the cornerstone of effective long-term management.