Vertigo is a disorienting condition characterized by the false sensation of spinning or motion. It stems primarily from dysfunction in the vestibular system, which includes the inner ear and parts of the brain responsible for balance. Contrary to common belief, vertigo is not a disease itself but rather a symptom of various underlying medical conditions.
Types of Vertigo and Their Underlying Causes
Benign Paroxysmal Positional Vertigo (BPPV)
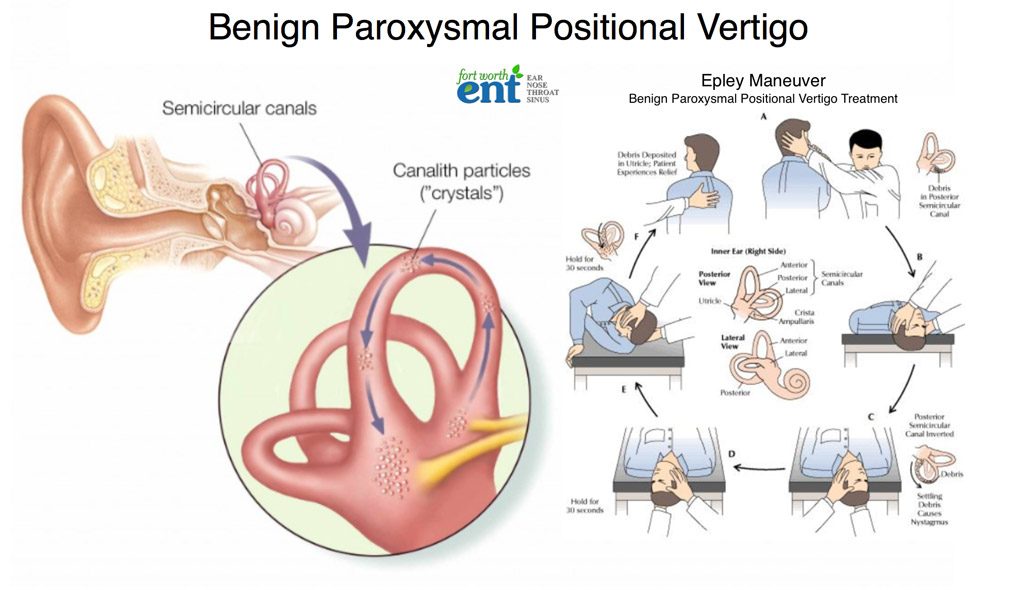
BPPV is the most prevalent form of vertigo, triggered by specific head movements. It results from the displacement of tiny calcium carbonate crystals (otoconia) within the semicircular canals of the inner ear, disrupting balance signals to the brain.
Meniere’s Disease
This chronic inner ear disorder involves fluid buildup in the labyrinth, leading to episodes of vertigo, tinnitus (ringing in the ears), fluctuating hearing loss, and aural fullness. The cause is not fully understood, but it may involve autoimmune, genetic, or viral factors.
Vestibular Neuritis and Labyrinthitis
Both conditions are linked to viral infections affecting the vestibular nerve or the labyrinth, respectively. They result in sudden, severe vertigo, often accompanied by nausea, vomiting, and difficulty with balance. Labyrinthitis may also affect hearing.
Central Vertigo
This originates from problems in the brainstem or cerebellum, commonly due to stroke, multiple sclerosis, tumors, or migraine. Unlike peripheral vertigo, central vertigo often includes additional neurological symptoms like double vision, slurred speech, or weakness.
Common Symptoms Associated with Vertigo
- Sensation of spinning, tilting, or swaying
- Loss of balance or unsteadiness
- Nausea and vomiting
- Abnormal eye movements (nystagmus)
- Headaches
- Tinnitus or hearing changes
Symptoms can vary in intensity and duration, ranging from seconds to hours or longer, depending on the cause.
Diagnostic Approaches for Vertigo
Physical Examination and History
A thorough clinical history is essential for identifying vertigo triggers and associated symptoms. Examination includes assessment of eye movements and balance.
Dix-Hallpike Maneuver
Used specifically to diagnose BPPV, this positional test evaluates for nystagmus and dizziness when the head is placed in specific angles.
Audiometric Tests
Hearing tests help distinguish between peripheral and central causes, especially in Meniere’s disease or labyrinthitis.
Imaging Studies
Magnetic Resonance Imaging (MRI) or Computed Tomography (CT) scans are employed to detect central causes such as stroke or tumor.
Vestibular Function Tests
Electronystagmography (ENG) or videonystagmography (VNG) measures involuntary eye movements. Vestibular evoked myogenic potentials (VEMP) assess inner ear function.
Treatment Options for Vertigo
Vestibular Rehabilitation Therapy (VRT)
This physical therapy aims to retrain the brain to interpret balance signals accurately. It is particularly effective in cases of unilateral vestibular loss or chronic imbalance.
Canalith Repositioning Maneuvers
For BPPV, maneuvers such as the Epley procedure reposition dislodged otoconia back into the utricle, alleviating symptoms in most cases.
Medications
- Antihistamines (e.g., meclizine) for acute vertigo episodes
- Benzodiazepines (e.g., diazepam) for short-term relief
- Antiemetics (e.g., promethazine) for nausea
- Diuretics and low-sodium diet for Meniere’s disease
- Steroids or antivirals for vestibular neuritis
Long-term medication is not advised unless vertigo is recurrent and unresponsive to other therapies.
Surgical Intervention
Reserved for severe or persistent cases, such as:
- Labyrinthectomy or vestibular nerve section
- Endolymphatic sac decompression in Meniere’s disease
- Removal of acoustic neuromas in central vertigo
Preventing Vertigo Recurrence
- Avoid sudden head movements
- Use extra caution when changing positions
- Stay hydrated and maintain a low-sodium diet
- Manage underlying conditions like hypertension and migraines
- Avoid triggers such as stress, alcohol, and bright lights
Vertigo in Special Populations
Elderly Individuals
Vertigo significantly increases the risk of falls and injuries in older adults. Multi-sensory decline and comorbidities complicate diagnosis and treatment. VRT and environmental modifications are crucial.
Pregnant Women
Hormonal changes, fluid retention, and increased sensitivity to motion contribute to vertigo during pregnancy. Non-pharmacological interventions are preferred to avoid fetal risk.
Children
Though less common, vertigo in children is often related to migraines or viral infections. Careful diagnosis and child-specific therapies are required.
Complications and When to Seek Immediate Care
While vertigo is typically benign, it may indicate a serious underlying condition if accompanied by:
- Sudden severe headache
- Difficulty speaking or walking
- Weakness or numbness
- Loss of consciousness
Immediate medical evaluation is essential in such scenarios.
Prognosis and Quality of Life
Most cases of vertigo resolve with appropriate diagnosis and treatment. However, recurrence is possible, particularly with BPPV or Meniere’s disease. Adherence to treatment and preventive strategies can significantly improve quality of life.
Frequently Asked Questions:
What is the main cause of vertigo?
The most common cause is Benign Paroxysmal Positional Vertigo (BPPV), where dislodged ear crystals interfere with balance signals.
Can vertigo go away on its own?
Yes, especially in mild cases. However, persistent or recurrent vertigo may require treatment and evaluation.
Is vertigo a sign of a serious condition?
While often benign, vertigo can sometimes indicate serious neurological conditions and warrants medical evaluation if accompanied by alarming symptoms.
How is vertigo different from dizziness?
Vertigo is a specific type of dizziness characterized by a spinning sensation, while general dizziness can include lightheadedness or imbalance without rotation.
Can stress or anxiety cause vertigo?
Yes, stress and anxiety can exacerbate or mimic vertigo, especially in individuals with vestibular disorders.
Vertigo is a complex, multifactorial symptom that significantly affects daily life and function. A comprehensive understanding of its causes, diagnosis, and treatment empowers individuals to manage and recover from this condition effectively. With appropriate care, most people can expect substantial improvement or complete resolution of symptoms.

