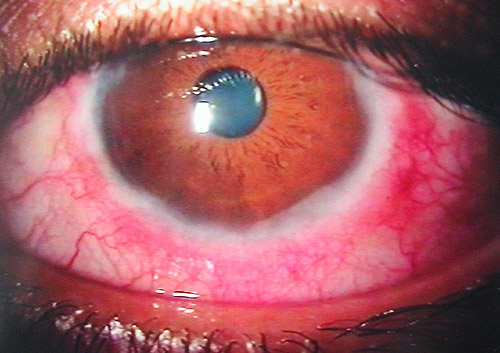
Vernal conjunctivitis, also known as vernal keratoconjunctivitis (VKC), is a recurrent, bilateral, and chronic allergic eye disorder predominantly affecting children and adolescents. It is most common in warm, dry climates and tends to intensify in the spring and summer, hence the term “vernal.” VKC is a severe form of allergic conjunctivitis characterized by conjunctival inflammation and corneal involvement, often leading to significant discomfort and potential vision impairment if not managed appropriately.
Epidemiology and Risk Factors
VKC is more prevalent in males under the age of 20, with onset typically between 5 and 15 years. It is rare in colder climates and shows strong seasonal variation. Several risk factors contribute to the development and exacerbation of VKC:
- Genetic predisposition: Family history of atopic conditions like asthma, eczema, or allergic rhinitis.
- Environmental exposure: Increased incidence in dry, hot, and windy regions.
- Hormonal influence: Symptoms often subside after puberty.
Pathophysiology and Immune Mechanisms
Vernal conjunctivitis involves a Type I (immediate) and Type IV (delayed) hypersensitivity reaction. Mast cells, eosinophils, and T-lymphocytes play key roles in the inflammatory cascade that leads to conjunctival and corneal damage.
Clinical Types of Vernal Conjunctivitis
1. Palpebral VKC
Characterized by large, cobblestone-like papillae on the upper tarsal conjunctiva. These “giant papillae” can cause mechanical irritation of the cornea.
2. Limbal VKC
Dominant in African populations, limbal VKC presents with gelatinous thickening at the limbus and Horner-Trantas dots—collections of eosinophils at the limbal area.
3. Mixed VKC
Features of both palpebral and limbal forms coexist in this subtype, often indicating more severe disease.
Common Symptoms of Vernal Conjunctivitis
- Intense ocular itching
- Tearing and photophobia
- Mucous discharge
- Sensation of foreign body
- Burning or stinging eyes
- Eyelid thickening or drooping
- Blurred vision in advanced stages due to corneal involvement
Diagnostic Criteria and Clinical Evaluation
Slit Lamp Examination
- Papillae: Especially on the upper tarsal conjunctiva.
- Trantas dots: White limbal dots formed by eosinophilic accumulation.
- Corneal involvement: Shield ulcers or punctate epithelial keratitis.
Conjunctival Scrapings
Reveals eosinophils, which support allergic etiology.
Differential Diagnoses
- Seasonal allergic conjunctivitis
- Atopic keratoconjunctivitis
- Bacterial or viral conjunctivitis
- Giant papillary conjunctivitis (e.g., contact lens wearers)
Treatment Options for Vernal Conjunctivitis
Environmental and Allergen Avoidance
- Limit exposure to wind, dust, and high pollen areas.
- Use sunglasses outdoors and keep windows closed during high pollen seasons.
Pharmacological Management
1. Antihistamines
- Olopatadine, azelastine – dual-action as antihistamine and mast cell stabilizers.
2. Mast Cell Stabilizers
- Lodoxamide, nedocromil – for long-term control and prevention of flare-ups.
3. Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- Ketorolac – useful in mild to moderate cases for reducing inflammation.
4. Corticosteroids
Reserved for acute exacerbations or severe symptoms. Use with caution to prevent side effects such as increased intraocular pressure and cataract formation.
- Loteprednol, fluorometholone – safer options for long-term use.
5. Immunomodulators
- Cyclosporine A 0.05% – effective for chronic cases unresponsive to steroids.
- Tacrolimus ointment – off-label but proven efficacy in severe VKC.
Surgical Intervention
Indicated in persistent shield ulcers or severe papillary hypertrophy:
- Superficial keratectomy
- Papillae excision
- Amniotic membrane transplantation
Complications of Vernal Conjunctivitis
- Corneal scarring and ulceration (shield ulcers)
- Visual impairment due to keratopathy
- Secondary infections
- Steroid-induced glaucoma or cataract with prolonged use
Prognosis and Long-Term Outcomes
VKC often resolves spontaneously after puberty. However, chronic or poorly managed cases can lead to significant morbidity. With appropriate treatment and monitoring, most patients achieve satisfactory control of symptoms.
Preventive Strategies
- Annual ophthalmological evaluations
- Use of hypoallergenic eye drops and lubricants
- Avoidance of eye rubbing to minimize mechanical trauma
- Early initiation of therapy at symptom onset
- Parental education for pediatric cases
Vernal conjunctivitis is a chronic and potentially sight-threatening allergic eye condition that requires a proactive and comprehensive management strategy. Early diagnosis, allergen control, and a tailored pharmacologic regimen are essential for symptom control and the prevention of complications. Advanced therapies like immunomodulators and surgical options offer promising outcomes for severe or refractory cases. With vigilant follow-up and preventive care, patients with VKC can maintain optimal visual health and quality of life.