Atrial fibrillation (AFib) is the most common sustained cardiac arrhythmia encountered in clinical practice. In patients with AFib, controlling the ventricular rate is a fundamental therapeutic goal aimed at alleviating symptoms, preventing tachycardia-induced cardiomyopathy, and improving overall cardiovascular outcomes. Ventricular rate control refers to the regulation of the rapid and irregular ventricular response that characterizes this arrhythmia.
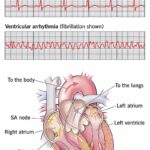
Mechanism of Rapid Ventricular Response in Atrial Fibrillation
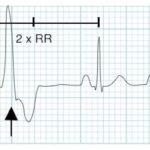
In AFib, the atria generate disorganized electrical impulses at rates of 300–600 beats per minute. These impulses bombard the atrioventricular (AV) node, which filters them before transmitting to the ventricles. Without proper control, this can result in a ventricular rate exceeding 100 bpm at rest, leading to hemodynamic compromise.
Goals of Ventricular Rate Control in Atrial Fibrillation
- Symptom Relief: Reduce palpitations, fatigue, and dyspnea.
- Prevent Tachycardia-Mediated Cardiomyopathy: Prolonged rapid ventricular rates impair left ventricular function.
- Improve Exercise Tolerance and Quality of Life: Especially crucial in active and elderly patients.
- Facilitate Left Ventricular Recovery: In patients with impaired systolic function.
- Prevent Hospitalizations: Particularly for acute heart failure or uncontrolled tachyarrhythmia.
Target Heart Rate in Rate Control Strategy
There are two approaches to target heart rate:
1. Strict Rate Control
- Goal: Resting heart rate <80 bpm and <110 bpm during moderate exertion
- Recommended for patients with persistent symptoms despite lenient control
2. Lenient Rate Control
- Goal: Resting heart rate <110 bpm
- Suitable for asymptomatic patients with preserved left ventricular function
Clinical trials, such as the RACE II study, have shown that lenient control is non-inferior to strict control in most patients, reducing the need for aggressive pharmacologic intervention.
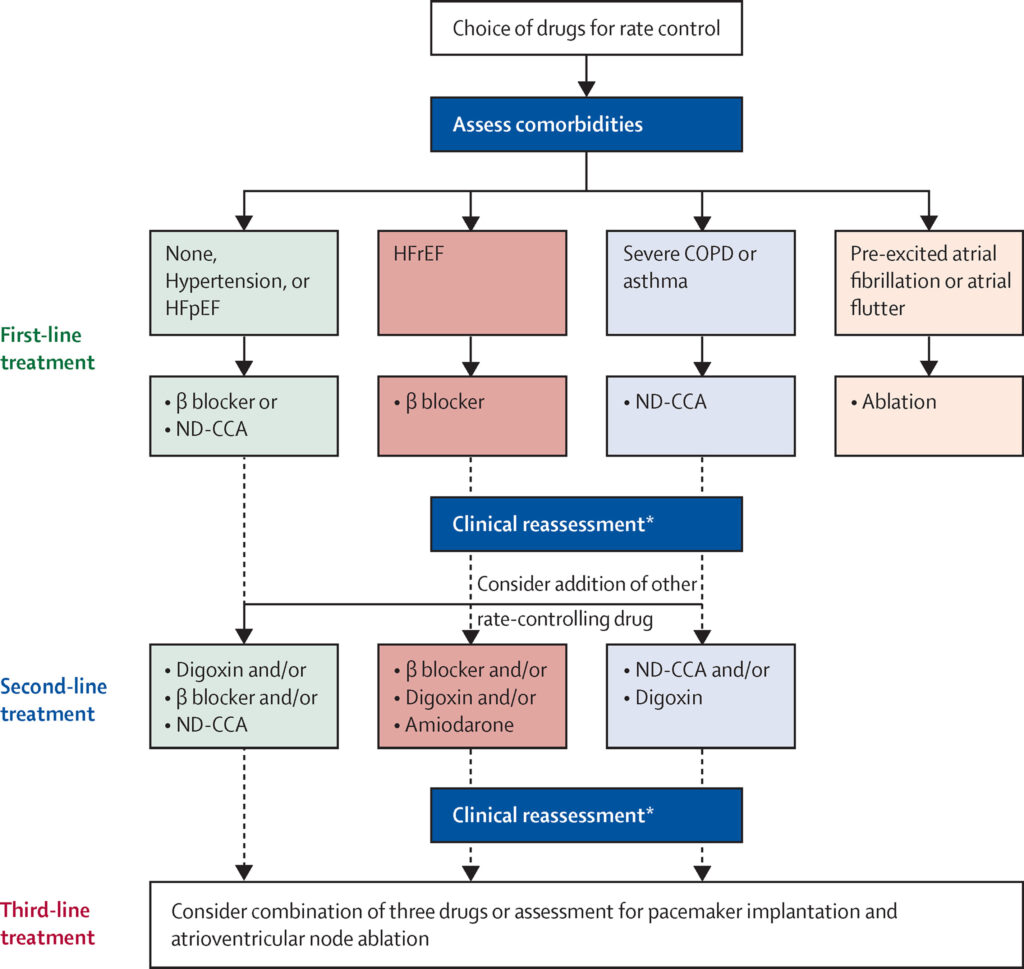
Pharmacological Agents for Ventricular Rate Control
1. Beta-Blockers
- Examples: Metoprolol, Atenolol, Bisoprolol, Carvedilol
- Mechanism: Decrease sympathetic tone, prolong AV nodal conduction
- Indications: First-line therapy in AFib, especially with coronary artery disease or heart failure with reduced ejection fraction (HFrEF)
Dosing Example:
- Metoprolol tartrate: 25–100 mg twice daily
- Metoprolol succinate (XL): 50–200 mg once daily
2. Non-Dihydropyridine Calcium Channel Blockers
- Examples: Diltiazem, Verapamil
- Mechanism: Block L-type calcium channels in the AV node, slowing conduction
- Indications: Effective in patients without HFrEF
Contraindications: Avoid in patients with left ventricular systolic dysfunction due to negative inotropic effects.
3. Digoxin
- Mechanism: Enhances vagal tone, reduces AV node conduction
- Indications: Resting rate control in sedentary or elderly patients, and in heart failure with reduced ejection fraction
Limitations: Less effective during exertion; narrow therapeutic index.
4. Amiodarone (Off-label for Rate Control)
- Use Case: In refractory cases or when rate control is urgent, particularly in critically ill patients or when other agents are contraindicated
Risks: Long-term toxicity includes thyroid, pulmonary, and hepatic complications.
Acute Rate Control in Hemodynamically Unstable Patients
In cases of rapid AFib with hypotension, angina, or acute heart failure, immediate rate control or cardioversion is warranted:
Intravenous Agents:
- Diltiazem: 0.25 mg/kg IV bolus over 2 minutes, followed by infusion
- Metoprolol: 2.5–5 mg IV bolus over 2 minutes, repeatable every 5 minutes
- Amiodarone: 150 mg IV bolus over 10 minutes, then continuous infusion
In cases where drug therapy is ineffective or contraindicated, electrical cardioversion may be required.
Long-Term Management Strategy: Rate vs Rhythm Control
While rate control is often sufficient, rhythm control may be considered in the following scenarios:
- Persistent symptoms despite adequate rate control
- Younger patients with paroxysmal AFib
- AFib-related cardiomyopathy not responsive to rate control
However, the choice between rate and rhythm control should be individualized based on patient characteristics, comorbidities, and treatment response.
Device Therapy and Invasive Options
1. Atrioventricular Node Ablation with Pacemaker Implantation
- Considered in patients with refractory AFib and uncontrolled ventricular rates
- Ablation of AV node followed by permanent pacemaker to ensure regular ventricular rhythm
Risks: Permanent pacemaker dependence, potential need for cardiac resynchronization therapy (CRT) in patients with LV dysfunction
Special Considerations in Rate Control
Elderly Patients
- Increased sensitivity to medications
- Prefer agents with a lower risk of hypotension or bradycardia
Patients with Heart Failure
- Beta-blockers preferred due to survival benefit
- Avoid verapamil and diltiazem in reduced LVEF
Athletes
- Resting bradycardia common
- Careful monitoring required when initiating rate control medications
Summary of Pharmacologic Choices Based on Patient Characteristics
| Clinical Scenario | Preferred Agent(s) |
|---|---|
| Heart failure with reduced EF | Beta-blockers, Digoxin |
| Hypertension or no LV dysfunction | Beta-blockers, Diltiazem, Verapamil |
| Coronary artery disease | Beta-blockers |
| Sedentary elderly patient | Digoxin |
| Acute rate control needed | IV Beta-blockers, Diltiazem, Amiodarone |
Effective ventricular rate control is essential in the management of atrial fibrillation to alleviate symptoms, prevent cardiomyopathy, and improve overall outcomes. A patient-centric approach, guided by clinical status and comorbidities, allows for tailored pharmacologic and interventional strategies. Early and appropriate management enhances quality of life and minimizes long-term complications associated with uncontrolled ventricular rates.