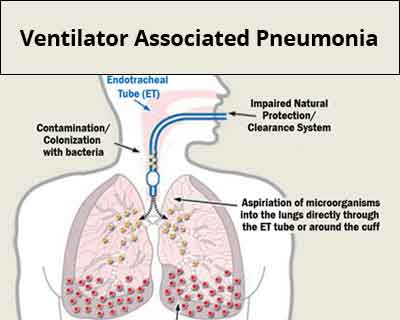
Ventilator-associated bacterial pneumonia (VABP) is a serious and potentially life-threatening infection that occurs in patients receiving mechanical ventilation for at least 48 hours. As a subtype of hospital-acquired pneumonia (HAP), VABP significantly contributes to morbidity, mortality, prolonged intensive care unit (ICU) stays, and increased healthcare costs.
Pathogenesis and Risk Factors of VABP
VABP develops when pathogenic bacteria colonize the lower respiratory tract through endotracheal intubation. The endotracheal tube impairs mucociliary clearance and acts as a conduit for pathogens, facilitating direct access to the lungs.
Key Risk Factors:
- Duration of mechanical ventilation
- Re-intubation or prolonged intubation
- Supine positioning
- Sedation and neuromuscular blockade
- Inadequate oral hygiene
- Prior antibiotic use
- Comorbidities such as diabetes or chronic lung disease
Common Pathogens in VABP
VABP is commonly caused by aerobic gram-negative bacilli and gram-positive cocci. Many cases involve multidrug-resistant (MDR) organisms, especially in long-term ICU stays.
Frequently Isolated Pathogens:
- Pseudomonas aeruginosa
- Acinetobacter baumannii
- Klebsiella pneumoniae
- Escherichia coli
- Staphylococcus aureus (including MRSA)
- Enterobacter spp.
These pathogens exhibit resistance mechanisms such as extended-spectrum beta-lactamases (ESBLs), carbapenemases, and methicillin resistance.
Clinical Presentation and Diagnostic Criteria
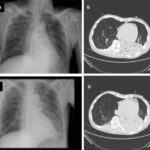
VABP presents with new or progressive radiographic infiltrates plus at least two of the following:
- Fever >38°C or hypothermia <36°C
- Leukocytosis or leukopenia
- Purulent tracheal secretions
- Hypoxia or worsening oxygenation
Diagnostic Approaches:
- Chest X-ray or CT scan: Essential for identifying new infiltrates.
- Microbiological testing:
- Endotracheal aspirates
- Bronchoalveolar lavage (BAL)
- Protected specimen brush (PSB)
- Blood cultures and inflammatory markers: CRP, procalcitonin, and complete blood count.
Antimicrobial Treatment Strategies
Empirical Therapy
Initiation of broad-spectrum antibiotics is essential within the first hour of clinical suspicion, especially in high-risk patients.
Recommended empiric regimens typically include:
- Anti-pseudomonal β-lactam (e.g., piperacillin-tazobactam, cefepime, meropenem)
- Plus MRSA coverage (e.g., vancomycin or linezolid)
- Dual anti-pseudomonal coverage may be required in settings with high MDR prevalence.
De-escalation and Targeted Therapy
Therapy should be narrowed based on culture results and antimicrobial susceptibility. De-escalation minimizes toxicity, resistance, and healthcare costs.
Duration of therapy: 7 days is generally adequate unless complications or poor clinical response are observed.
Role of Antibiotic Stewardship
Effective antibiotic stewardship ensures optimal antimicrobial use by:
- Monitoring resistance patterns
- Reducing unnecessary broad-spectrum antibiotic use
- Promoting timely de-escalation
- Implementing local antibiograms for empirical selection
Prevention and Infection Control Measures
Ventilator Care Bundle Strategies:
- Elevate head of bed 30°–45°
- Daily sedation vacation and assessment of readiness to extubate
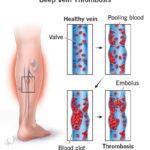
- Peptic ulcer disease and deep vein thrombosis prophylaxis
- Oral care with chlorhexidine
- Subglottic secretion drainage
Additional Measures:
- Hand hygiene adherence
- Sterile suctioning techniques
- Minimizing circuit changes unless visibly soiled
- Using closed suction systems when possible
Emerging Therapies and Future Directions
- Inhaled antibiotics (e.g., aerosolized aminoglycosides, colistin) for MDR VABP
- Rapid molecular diagnostics to identify pathogens and resistance genes
- Monoclonal antibodies and bacteriophage therapy under research
- AI-based surveillance systems to detect early signs of VABP
Prognosis and Outcomes
Outcomes in VABP are highly variable and depend on:
- Timeliness and appropriateness of antibiotic therapy
- Pathogen virulence and resistance profile
- Patient comorbidities and immune status
Mortality rates range from 20% to 50% in critically ill populations. Early intervention and adherence to prevention protocols are crucial to improving survival and reducing ICU stay duration.
Ventilator-associated bacterial pneumonia remains a critical concern in intensive care settings due to its significant clinical and economic impact. Early recognition, prompt targeted therapy, and rigorous preventive measures form the cornerstone of effective VABP management. Integration of novel diagnostics and stewardship programs enhances clinical outcomes and helps curb antimicrobial resistance.