Vasomotor symptoms (VMS), most commonly experienced as hot flashes and night sweats, are hallmark signs of the menopausal transition. These symptoms stem from hormonal changes, primarily the declining levels of estrogen, which disrupt the body’s thermoregulation.
VMS affect approximately 75% of menopausal women, with varying intensity and duration. For some, these symptoms are mild and short-lived, while others endure severe episodes that significantly impair quality of life and sleep.
The Physiology of Hot Flashes and Night Sweats
Hot flashes are sudden, intense sensations of heat, often starting in the chest or face and radiating throughout the body. Night sweats are the nocturnal counterpart, frequently disrupting sleep cycles.
These phenomena are caused by the hypothalamus, the brain’s temperature control center, becoming more sensitive due to estrogen deficiency. The narrowing of the thermoneutral zone prompts the body to overreact to minor temperature changes.
Key Characteristics of Vasomotor Symptoms
| Symptom | Description | Duration |
|---|---|---|
| Hot Flashes | Intense warmth, flushing, sweating | 30 sec to 5 mins |
| Night Sweats | Profuse sweating during sleep | Disruptive to REM |
| Chills/Cold Sweats | May follow hot flashes | Transient |
| Sleep Disturbances | Secondary to night sweats | Chronic in severe cases |
Risk Factors Influencing Severity and Duration
Several factors may influence the onset, frequency, and intensity of vasomotor symptoms.
Biological and Lifestyle Risk Factors
- Early menopause or surgical removal of ovaries
- Higher BMI increases symptom severity
- Smoking associated with earlier and more intense VMS
- Stress and anxiety worsen symptom perception
- Genetics may predispose some individuals to longer durations
Duration of Symptoms
While VMS were once thought to last only a few years, research shows they can persist for 7–10 years or more, with some women experiencing symptoms into their 70s.
Diagnosing Vasomotor Symptoms During Menopausal Transition
Diagnosis is primarily clinical, based on reported symptoms in perimenopausal or postmenopausal women. Laboratory tests are not typically required unless there is uncertainty about the menopausal status.
Key indicators include:
- Irregular or ceased menstruation
- Typical VMS without identifiable alternative causes
- Age range between 45–55 years
Exclusion of hyperthyroidism, carcinoid syndrome, and other differential diagnoses is important when symptoms are atypical or begin before age 40.
Hormone Therapy: The Most Effective VMS Treatment
Estrogen-Based Therapies
Hormone therapy (HT) is the gold standard for managing moderate to severe vasomotor symptoms. It replenishes declining estrogen levels, thereby stabilizing thermoregulatory control.
- Estrogen-only therapy: For women without a uterus
- Combined estrogen-progestin therapy: For women with an intact uterus to prevent endometrial hyperplasia
Benefits:
- Reduces frequency and intensity of hot flashes by up to 80%
- Improves sleep quality and mood
- May have protective cardiovascular effects when initiated early in menopause
Risks and Considerations
Long-term HT is associated with increased risks of:
- Breast cancer (with combined therapy)
- Blood clots and stroke (especially in older users)
Therefore, HT should be prescribed at the lowest effective dose for the shortest duration, tailored to the individual.
Non-Hormonal Treatments for Vasomotor Symptoms
For those who cannot or choose not to use hormone therapy, several non-hormonal options offer relief.
FDA-Approved Non-Hormonal Drug Options
| Medication | Class | Mechanism |
|---|---|---|
| Paroxetine (Brisdelle) | SSRI | Modifies serotonin to stabilize thermoregulation |
| Gabapentin | Anticonvulsant | Reduces nighttime VMS |
| Clonidine | Alpha-agonist | Lowers central sympathetic outflow |
| Fezolinetant | NK3 receptor antagonist | Blocks neurokinin B pathways linked to hot flashes |
Complementary Approaches
- Cognitive Behavioral Therapy (CBT): Reduces distress and improves symptom coping
- Mindfulness & Yoga: Shown to decrease VMS severity and improve sleep
- Acupuncture: Mixed evidence but may offer symptom relief for some
- Herbal Supplements: Black cohosh and phytoestrogens (e.g., soy isoflavones) have anecdotal benefits, though clinical evidence is limited
Lifestyle Modifications to Reduce Vasomotor Symptoms
Strategic lifestyle adjustments can substantially ease the burden of VMS.
Practical Tips
- Wear lightweight, breathable clothing
- Use cooling fans and maintain ambient room temperature
- Avoid spicy foods, alcohol, and caffeine
- Engage in regular physical activity
- Maintain a healthy weight
- Practice stress reduction techniques such as meditation or journaling
Long-Term Impacts of Untreated Vasomotor Symptoms
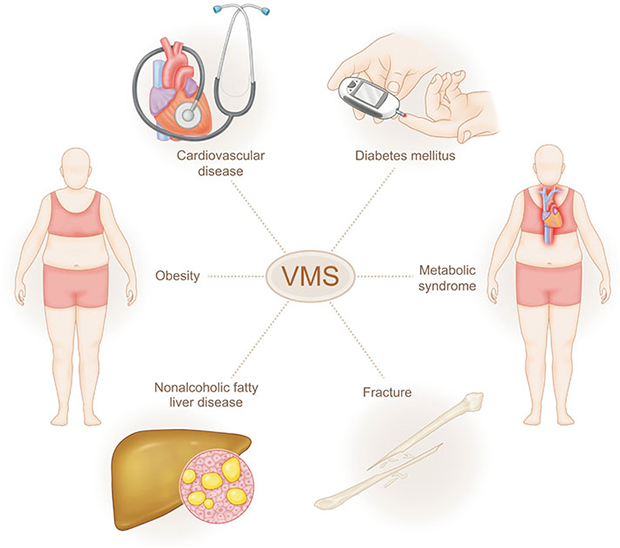
Chronic VMS are more than discomfort — they are associated with:
- Insomnia and poor sleep quality
- Depressive symptoms and anxiety
- Impaired cognitive function
- Reduced work productivity and social functioning
Women with persistent hot flashes may also face elevated cardiovascular risks, underscoring the importance of proper evaluation and treatment.
Frequently Asked Questions:
What are vasomotor symptoms in menopause?
Vasomotor symptoms refer to hot flashes and night sweats caused by estrogen withdrawal during the menopausal transition.
How long do vasomotor symptoms last?
VMS can last anywhere from a few months to over a decade. On average, they persist for 7–10 years.
Can vasomotor symptoms occur in perimenopause?
Yes. In fact, symptoms often begin during perimenopause, even before menstrual periods cease entirely.
What is the most effective treatment for vasomotor symptoms?
Hormone therapy is the most effective treatment, particularly estrogen-based regimens tailored to individual risk profiles.
Are there natural remedies that work?
Some women find relief through lifestyle changes, CBT, herbal remedies, and practices like yoga, though results vary.
Vasomotor symptoms are among the most disruptive manifestations of menopause, significantly affecting well-being and quality of life. With a range of effective treatments—from hormone therapy to non-hormonal and behavioral strategies—personalized management is both achievable and essential. We advocate for proactive evaluation and tailored interventions to empower women through the menopausal journey with resilience and confidence.