Vascular access thrombosis is a significant complication in patients undergoing hemodialysis. It involves the formation of a blood clot within the vascular access site, such as an arteriovenous (AV) fistula, AV graft, or central venous catheter. The condition is a leading cause of vascular access failure, contributing to increased morbidity, hospitalization rates, and health care costs.
Prompt diagnosis, effective intervention, and preventive strategies are essential to maintain long-term access patency and ensure uninterrupted dialysis treatment.
Types of Vascular Access and Thrombosis Risk
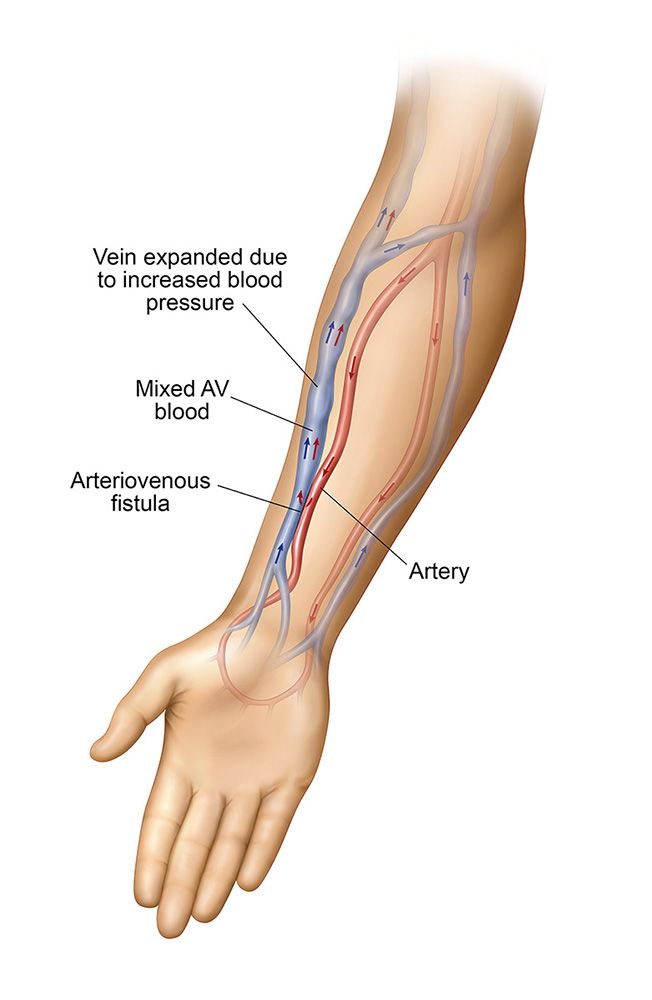
1. Arteriovenous Fistula (AVF) Thrombosis
AV fistulas are the preferred vascular access for long-term hemodialysis due to their lower infection and thrombosis rates. However, thrombosis may occur, especially in cases of underlying stenosis or repeated trauma.
Common Causes:
- Juxta-anastomotic stenosis
- Repeated needle punctures
- Low flow due to hypotension or dehydration
2. Arteriovenous Graft (AVG) Thrombosis
AV grafts are synthetic conduits connecting an artery to a vein and have higher thrombosis rates compared to AVFs due to intimal hyperplasia and stenosis at anastomotic sites.
Common Causes:
- Neointimal hyperplasia
- Inflammatory response to synthetic material
- Venous outflow obstruction
3. Central Venous Catheter (CVC) Thrombosis
CVCs are used for immediate access but are highly susceptible to thrombotic complications due to their intravascular placement and turbulent blood flow.
Common Causes:
- Catheter tip malposition
- Fibrin sheath formation
- Venous stenosis or endothelial injury
Pathophysiology of Access Thrombosis
Vascular access thrombosis results from an interplay of mechanical and hemodynamic factors:
- Endothelial injury: Repeated cannulation or synthetic graft exposure
- Venous stenosis: Promotes turbulence and platelet activation
- Stasis of blood flow: Hypotension or access compression
- Hypercoagulable states: Uremia, inflammation, malignancy
These factors align with Virchow’s triad—stasis, vessel wall injury, and hypercoagulability—leading to thrombus formation and occlusion of the access site.
Clinical Presentation and Diagnosis
Symptoms and Signs
- Sudden loss of thrill or bruit over access site
- Decreased dialysis adequacy (Kt/V, urea reduction ratio)
- Swelling or erythema of limb
- Inability to cannulate or aspirate blood from the access
- Increased venous pressures during dialysis
Diagnostic Evaluation
- Physical Examination
- Palpation for thrill
- Auscultation for bruit
- Duplex Ultrasound
- Identifies thrombus and evaluates flow dynamics
- Detects stenosis and venous outflow obstruction
- Angiography
- Gold standard for identifying stenosis and thrombus
- Allows for concurrent intervention (angioplasty or thrombectomy)
- Venography (for CVCs)
- Visualizes central vein patency
- Assesses catheter tip location and fibrin sheath
Treatment of Vascular Access Thrombosis
Thrombosed AV Fistulas and Grafts
Endovascular Options:
- Percutaneous Mechanical Thrombectomy
- Devices fragment and aspirate thrombus
- Pharmacomechanical Thrombolysis
- Use of thrombolytic agents (tPA) with mechanical removal
- Balloon Angioplasty (PTA)
- Treats underlying stenosis post-thrombectomy
- Stent Placement
- For recurrent or resistant stenosis
Surgical Options:
- Thrombectomy with access revision
- Graft interposition or patch angioplasty
- New access creation if salvage fails
Catheter-Related Thrombosis
- Thrombolytic Lock Therapy
- Instillation of alteplase into catheter lumen
- Catheter Exchange or Removal
- If clot is extensive or fibrin sheath cannot be lysed
- Anticoagulation
- Heparin or direct oral anticoagulants (DOACs) for systemic involvement
Prevention Strategies for Vascular Access Thrombosis
Optimizing Cannulation Technique
- Use of buttonhole technique for AVFs
- Proper needle gauge and insertion angle
- Rotating puncture sites to avoid vessel injury
Surveillance and Monitoring
- Access flow measurements (QA)
- Venous pressure monitoring during dialysis
- Routine ultrasound surveillance for early detection of stenosis
Pharmacologic Prophylaxis
- Antiplatelet agents (e.g., aspirin) in selected high-risk patients
- Anticoagulants rarely used for long-term prevention due to bleeding risk
Patient Education
- Encourage reporting of changes in thrill or swelling
- Educate on proper arm positioning and access protection
- Avoidance of constrictive clothing or sleeping on the access arm
Long-Term Outcomes and Access Salvage
Timely intervention can restore access patency in up to 80% of cases, particularly when performed within 48 hours of thrombosis. However, recurrent thrombosis increases the risk of permanent access loss. AVFs typically have better salvage outcomes than grafts.
Factors Impacting Prognosis
- Duration of access dysfunction
- Type of vascular access
- Presence of correctable underlying stenosis
- Patient comorbidities and vascular status
A multidisciplinary approach involving nephrologists, interventional radiologists, and vascular surgeons is key to optimizing outcomes.
Vascular access thrombosis poses a significant threat to dialysis adequacy and patient survival. Early recognition, prompt treatment, and ongoing surveillance are essential to prevent irreversible access loss. By understanding the pathogenesis, employing strategic interventions, and promoting proactive care, we can enhance vascular access longevity and improve the overall quality of hemodialysis therapy.