Vaginal cuff surgery is a critical component of a total hysterectomy, wherein the upper portion of the vagina is sutured following the removal of the uterus and cervix. This area, known as the vaginal cuff, is vulnerable to post-operative complications, particularly infections, which may arise due to microbial contamination, improper healing, or tissue necrosis. Vigilant care and prompt identification are essential to minimize morbidity.
Pathophysiology of Post-Operative Vaginal Cuff Infections
Post-operative infections following vaginal cuff surgery typically occur when pathogenic microorganisms colonize the surgical site. Factors such as tissue trauma, hematoma, devitalized tissue, and pre-existing vaginal or gastrointestinal flora increase the risk. The most common causative organisms include aerobic and anaerobic bacteria such as Escherichia coli, Bacteroides, Streptococcus, and Staphylococcus species.
Common Causes and Contributing Factors
- Surgical technique: Poor suture placement or contamination during procedure
- Compromised immune system: Diabetes, HIV, immunosuppressive therapy
- Bowel or bladder injury: Increases exposure to polymicrobial flora
- Poor vaginal hygiene post-surgery
- Delayed wound healing: Smoking, obesity, anemia, or malnutrition
Clinical Manifestations of Vaginal Cuff Post-Op Infections
Localized Symptoms
- Persistent pelvic or abdominal pain
- Foul-smelling or purulent vaginal discharge
- Vaginal bleeding beyond normal healing expectations
- Redness or swelling at the vaginal apex during examination
- Fever >100.4°F (38°C)
Systemic Signs
- Tachycardia and hypotension
- Fatigue and malaise
- Gastrointestinal symptoms: nausea, vomiting, bloating
- Signs of sepsis in advanced cases
Prompt medical assessment is essential to prevent escalation into systemic infection or abscess formation.
Diagnostic Evaluation for Vaginal Cuff Infection
Clinical Examination
A pelvic exam reveals erythema, tenderness, or discharge at the vaginal cuff. Speculum examination is crucial for visualizing dehiscence or purulence.
Laboratory Tests
- CBC with differential: Leukocytosis with neutrophilia
- CRP and ESR: Elevated inflammatory markers
- Vaginal swab culture: Identifies causative organisms
- Urinalysis: Rules out concurrent urinary tract infection
- Blood cultures: If systemic symptoms or sepsis is suspected
Imaging
- Transvaginal ultrasound: Detects pelvic fluid collections or hematomas
- CT scan of abdomen and pelvis: Evaluates abscesses or deep pelvic infections
Effective Management Strategies for Vaginal Cuff Infections
Initial Medical Therapy
Empirical broad-spectrum antibiotics are initiated and adjusted based on culture results. Common regimens include:
- Cefoxitin or Ceftriaxone + Metronidazole
- Clindamycin + Gentamicin for anaerobic and gram-negative coverage
- Ampicillin-sulbactam as monotherapy alternative
Antibiotic treatment is continued for 10–14 days, with IV-to-oral switch based on patient response.
Surgical Intervention
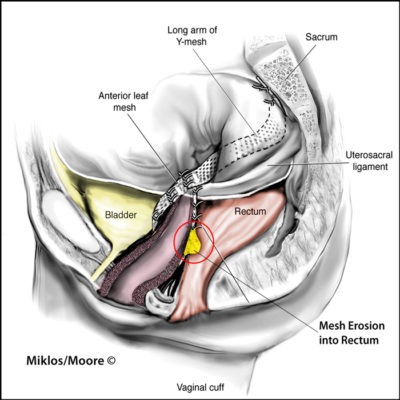
Surgical exploration or intervention is required when:
- Abscess formation is confirmed
- Cuff dehiscence with evisceration is observed
- Necrotic tissue necessitates debridement
- Conservative treatment fails
Procedures may include laparoscopic drainage, vaginal cuff revision, or removal of infected sutures.
Vaginal Cuff Dehiscence and Its Relationship with Infection
Dehiscence refers to the reopening of the sutured vaginal cuff. Infection is both a cause and consequence of this complication. Evisceration—protrusion of intra-abdominal contents through the vaginal canal—represents a surgical emergency.
Risk Factors for Dehiscence:
- Early resumption of sexual activity
- Increased intra-abdominal pressure
- Poor surgical technique
- Use of thermal energy devices
- Concurrent infection delaying healing
Prevention of Vaginal Cuff Surgery Infections
Preoperative Measures
- Antiseptic vaginal preparation
- Prophylactic antibiotic administration within 1 hour of incision
- Blood glucose control in diabetic patients
- Bowel preparation if contamination is likely
Intraoperative Measures
- Sterile technique and gentle tissue handling
- Minimizing electrocautery use at the cuff
- Adequate hemostasis to prevent hematoma
- Thorough irrigation before closure
Postoperative Care
- Educating the patient on wound care
- Advising sexual abstinence for 6–8 weeks
- Early detection of symptoms
- Routine follow-up within 2–3 weeks post-surgery
Recovery Timeline and Prognosis
With timely intervention, most vaginal cuff infections resolve without long-term complications. Full recovery typically takes 4–6 weeks, but may extend depending on severity, surgical revision, or systemic illness.
Patients must monitor for recurrent symptoms and adhere strictly to follow-up appointments, as delayed diagnosis can lead to chronic pelvic inflammatory disease, adhesions, or infertility in select cases.
Frequently Asked Questions
What is the most common symptom of a post-op vaginal cuff infection?
Persistent pelvic pain and unusual vaginal discharge are typically the earliest signs.
How soon can an infection appear after vaginal cuff surgery?
Infections usually manifest within 5–14 days post-surgery but may occur later.
Is a vaginal cuff infection life-threatening?
If left untreated, it can lead to sepsis or abscess formation, which are serious but preventable complications.
Can I prevent vaginal cuff infections after hysterectomy?
Yes. Following postoperative instructions, maintaining hygiene, and attending scheduled check-ups significantly reduce infection risk.
When should I seek immediate care?
Seek urgent evaluation for high fever, foul-smelling discharge, heavy bleeding, or abdominal pain after surgery.
Vaginal cuff surgery post-op infections, though relatively uncommon, require immediate attention due to their potential for serious complications. Understanding the signs, maintaining rigorous perioperative hygiene, and adhering to follow-up protocols are key in preventing infection and ensuring a smooth postoperative course. We advocate for comprehensive care, timely diagnosis, and targeted therapy to safeguard patient outcomes in gynecologic surgical recovery.