Vaginal cuff surgery, typically following a total hysterectomy, involves suturing the top portion of the vaginal canal after removal of the uterus. While usually successful, a major postoperative risk includes infectious complications—among which Clostridium species, particularly Clostridium difficile and Clostridium perfringens, present a rare but dangerous threat. These gram-positive, spore-forming anaerobes can lead to fulminant infections, tissue necrosis, and systemic toxicity.

Clostridium Infections: Pathogenesis in Post-Hysterectomy Cases
Clostridium species are part of the endogenous flora in the gastrointestinal and, occasionally, genital tract. Surgical procedures involving the uterus, bowel, or vagina can inadvertently introduce Clostridium into sterile sites. These bacteria thrive in hypoxic conditions, such as poorly perfused or necrotic tissue at the vaginal cuff, allowing for rapid toxin-mediated damage.
Common Clostridium Strains in Post-Op Infections
- Clostridium perfringens – Gas gangrene, myonecrosis
- Clostridium difficile – Pseudomembranous colitis, systemic sepsis
- Clostridium sordellii – Rare, associated with toxic shock-like syndrome
Clinical Presentation of Post-Op Clostridium Infections
Early Symptoms
- High fever (>39°C)
- Sudden onset pelvic pain
- Tachycardia and hypotension
- Malodorous vaginal discharge
- Abdominal distention
Advanced Complications
- Gas gangrene at vaginal cuff or pelvic site
- Toxic shock-like syndrome with multiorgan failure
- Sepsis with altered mental status
Timely recognition is vital, as mortality can escalate without rapid intervention.
Diagnostic Approach to Clostridium Infections After Vaginal Cuff Surgery
Laboratory Tests
- CBC: Elevated WBC with left shift
- Lactate & CRP: Markers of systemic infection and tissue hypoperfusion
- Blood cultures: To isolate anaerobes
- Toxin assay or PCR for C. difficile if diarrhea or colitis is suspected
Imaging Techniques
- CT Abdomen and Pelvis: Gas bubbles, abscess, or soft tissue swelling
- MRI with contrast: To assess necrotic involvement or fistula formation
Early imaging may show emphysematous changes at the vaginal cuff suggestive of Clostridium perfringens.
Medical and Surgical Management Strategies
Empiric Antimicrobial Therapy
Initiate broad-spectrum antibiotics immediately, then tailor based on culture results. Effective regimens include:
- Piperacillin-tazobactam
- Clindamycin (inhibits toxin production)
- Metronidazole (targeted for anaerobes)
- Vancomycin (oral) for suspected C. difficile colitis
Antibiotic duration: Minimum of 10–14 days, extended based on clinical response.
Surgical Interventions
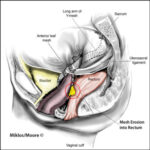
- Debridement of necrotic tissue at the vaginal cuff
- Laparoscopic or open drainage of abscesses
- Hysterectomy (if not already done) in severe cases of uterine infection
- Reconstruction or revision of the cuff after infection control
Preventive Strategies Against Clostridial Infections
Preoperative
- Proper bowel preparation when needed
- Antibiotic prophylaxis covering anaerobes (e.g., cefazolin + metronidazole)
- Screening for recent C. difficile infection or antibiotic use
Intraoperative
- Minimizing surgical time
- Maintaining aseptic technique
- Ensuring adequate perfusion to the vaginal cuff
Postoperative
- Early ambulation and hydration
- Monitoring for signs of infection
- Avoiding unnecessary antibiotic use to reduce C. difficile risk
Risk Factors for Developing Clostridium Infections Post-Surgery
| Risk Factor | Impact |
|---|---|
| Immunosuppression | Reduced infection control |
| Recent or prolonged antibiotic use | Risk of C. difficile overgrowth |
| Poor glycemic control | Impaired wound healing |
| Necrotic tissue at cuff site | Promotes anaerobic growth |
| Previous abdominal or pelvic surgery | Increased adhesions and compromised perfusion |
Long-Term Implications of Untreated Clostridial Infections
- Chronic pelvic pain
- Vaginal cuff fistula formation
- Recurrent abscesses
- Septic shock and death
- Adhesion-related bowel obstruction
Prompt treatment significantly reduces morbidity and improves surgical outcomes.
FAQs:
What is a Clostridium infection after vaginal cuff surgery?
It is a serious postoperative complication where anaerobic Clostridium bacteria infect the surgical site, leading to rapid tissue damage and systemic illness.
How is it different from typical post-op infections?
Clostridium infections produce potent toxins that cause faster and more destructive infections than common aerobic pathogens.
Is it curable?
Yes, with rapid diagnosis, appropriate antibiotics, and surgical debridement, most patients recover fully.
Can C. difficile infect the vaginal cuff?
While primarily an enteric pathogen, C. difficile can lead to systemic infection and may complicate gynecological surgeries through hematogenous spread or colonic translocation.
What are the warning signs?
Severe pelvic pain, fever, foul discharge, and signs of sepsis within days post-surgery warrant urgent medical evaluation.