Vulvar cancer is a rare but serious form of cancer that affects the external female genitalia. A significant proportion of vulvar cancer cases are attributed to persistent infection with high-risk types of the human papillomavirus (HPV), particularly HPV-16 and HPV-18. These oncogenic strains lead to cellular changes in the vulvar epithelium, increasing the risk of neoplastic transformation.

Role of HPV in Vulvar Cancer Pathogenesis
Human papillomavirus is a DNA virus that infects epithelial cells. Among the over 100 identified HPV types, approximately 14 are classified as high-risk for their ability to cause malignancies. In vulvar cancer, HPV DNA is frequently detected, particularly in younger women. HPV-induced vulvar neoplasia often begins as vulvar intraepithelial neoplasia (VIN), which, if left untreated, may progress to invasive carcinoma.
HPV Vaccination: A Critical Tool for Prevention
The introduction of prophylactic HPV vaccines has revolutionized cancer prevention strategies. These vaccines, particularly the nonavalent HPV vaccine (Gardasil 9), target multiple high-risk HPV types responsible for the majority of HPV-associated cancers, including vulvar cancer.
Available HPV Vaccines and Coverage
| Vaccine | HPV Types Covered | Cancer Prevention Coverage |
|---|---|---|
| Gardasil | 6, 11, 16, 18 | Cervical, vulvar, vaginal, anal |
| Gardasil 9 | 6, 11, 16, 18, 31, 33, 45, 52, 58 | Expanded coverage including 9 HPV types |
| Cervarix | 16, 18 | Effective against cervical and vulvar cancers |
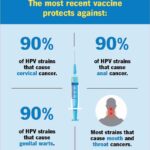
Gardasil 9 is currently the most comprehensive option, covering nearly 90% of HPV types linked to vulvar cancer.
Ideal Age and Schedule for HPV Vaccination
Recommended Vaccination Age
The Centers for Disease Control and Prevention (CDC) recommends routine HPV vaccination at:
- Ages 11–12: Optimal immune response and prior to potential HPV exposure
- Catch-up vaccination: For individuals up to age 26
- Adults aged 27–45: Based on shared clinical decision-making with healthcare providers
Dosing Schedule
| Age Group | Doses Required | Schedule |
|---|---|---|
| 9–14 years | 2 doses | 0 and 6–12 months |
| 15 years and up | 3 doses | 0, 1–2, and 6 months |
Efficacy of HPV Vaccination in Vulvar Cancer Prevention
Clinical trials and population-level studies have demonstrated the high efficacy of HPV vaccination in preventing HPV-associated VIN and subsequent vulvar cancer. Immunization has led to significant reductions in precancerous lesions, especially when administered before HPV exposure.
Evidence-Based Outcomes
- A study in The Lancet reported up to 97% efficacy against HPV-16/18-related high-grade VIN.
- Countries with high HPV vaccine coverage, such as Australia and Sweden, report drastic declines in HPV infections and associated lesions.
- Long-term surveillance confirms sustained immune protection lasting over a decade post-vaccination.
Safety and Side Effects of HPV Vaccines
HPV vaccines undergo rigorous safety evaluations. Common mild side effects include:
- Pain, swelling, or redness at the injection site
- Fever
- Fatigue
- Headache
Severe adverse effects are exceedingly rare. Global health authorities, including the World Health Organization (WHO), affirm the safety profile of HPV vaccines.
Addressing Vaccine Hesitancy
Despite proven benefits, misinformation and misconceptions contribute to vaccine hesitancy. Public health initiatives must emphasize:
- The non-sexual nature of prevention: HPV vaccination is cancer prevention
- Scientific consensus on safety and efficacy
- The importance of early vaccination for maximum protection
HPV Vaccination as a Public Health Imperative
Vaccination against HPV represents a cornerstone of modern cancer prevention. By preventing high-risk HPV infections, we can significantly reduce the incidence of vulvar cancer and other anogenital malignancies. Timely immunization, especially prior to exposure, ensures long-term protection and supports global efforts to eliminate HPV-associated cancers.