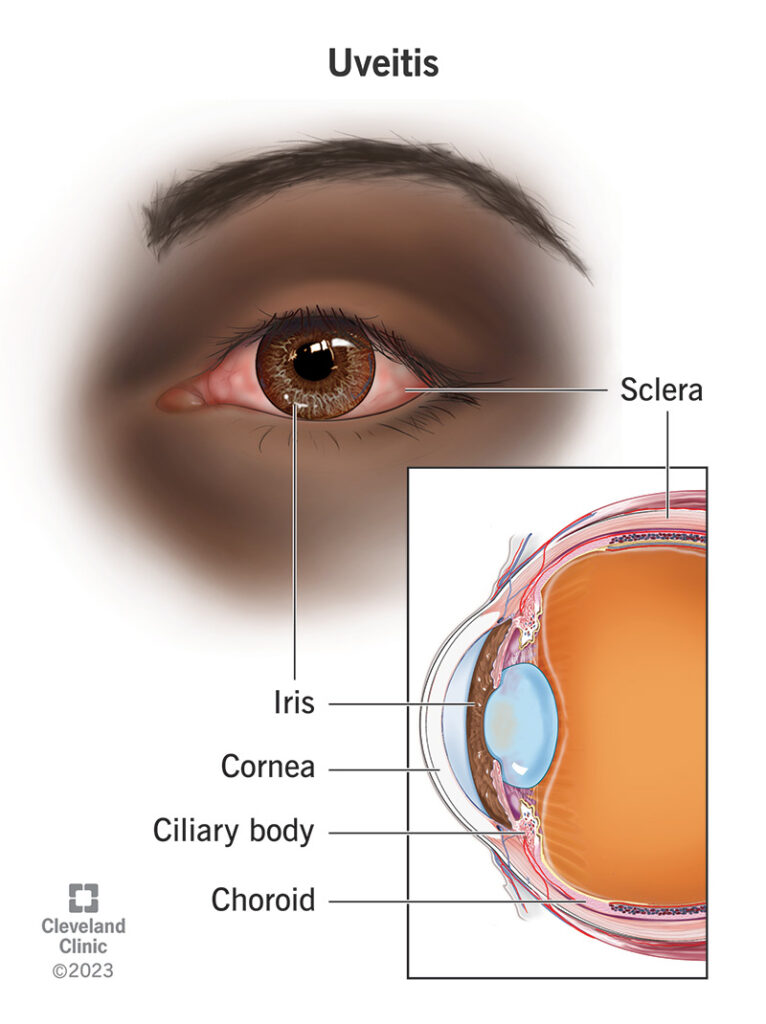
Uveitis refers to inflammation of the uvea, the middle layer of the eye, comprising the iris, ciliary body, and choroid. It plays a vital role in nourishing the retina and regulating light entry. Uveitis may also involve adjacent structures such as the retina, vitreous, and optic nerve, making early diagnosis and prompt treatment critical to prevent vision loss.
Classification of Uveitis by Anatomical Location
Anterior Uveitis (Iritis)
This is the most common form and affects the front part of the uvea, particularly the iris and anterior chamber. It may present acutely or chronically.
- Symptoms: Eye pain, redness, photophobia, blurred vision
- Common Causes: Autoimmune disorders (e.g., HLA-B27), trauma, infections
Intermediate Uveitis (Pars Planitis)
Affects the vitreous and the pars plana region of the ciliary body.
- Symptoms: Floaters, mild vision loss
- Associated Conditions: Multiple sclerosis, sarcoidosis, idiopathic
Posterior Uveitis
Involves the retina and choroid. It can significantly impair vision due to retinal inflammation.
- Symptoms: Visual field defects, floaters, decreased vision
- Causes: Toxoplasmosis, CMV, autoimmune diseases
Panuveitis
Characterized by inflammation of all uveal components. It is the most severe and may result in permanent visual damage.
- Symptoms: Severe vision loss, pain, photophobia
- Causes: Behçet’s disease, Vogt-Koyanagi-Harada (VKH) syndrome, sympathetic ophthalmia
Causes and Risk Factors of Uveitis
Uveitis can be idiopathic or secondary to a wide spectrum of systemic and ocular conditions. Identifying the underlying etiology is essential for targeted therapy.
Infectious Causes
- Bacterial: Tuberculosis, syphilis, Lyme disease
- Viral: Herpes simplex virus, cytomegalovirus, varicella-zoster
- Parasitic: Toxoplasma gondii
Autoimmune and Systemic Inflammatory Diseases
- HLA-B27 associated arthropathies
- Ankylosing spondylitis
- Behçet’s disease
- Juvenile idiopathic arthritis
- Sarcoidosis
- Systemic lupus erythematosus
Other Causes
- Trauma: Post-surgical or penetrating injuries
- Drug-induced: Rifabutin, bisphosphonates
- Malignancy: Intraocular lymphoma mimicking uveitis
Signs and Symptoms of Uveitis
The clinical presentation varies based on the anatomical location and duration of inflammation.
| Type | Key Symptoms |
|---|---|
| Anterior Uveitis | Redness, eye pain, photophobia, decreased visual acuity |
| Intermediate Uveitis | Floaters, mild blurring of vision |
| Posterior Uveitis | Floaters, vision loss, night blindness |
| Panuveitis | Severe pain, extensive visual impairment |
Common signs observed during slit-lamp and fundoscopic examination include:
- Anterior chamber cells and flare
- Keratic precipitates
- Hypopyon
- Vitritis
- Retinal vasculitis
- Chorioretinal lesions
Diagnostic Workup for Uveitis
An accurate diagnosis relies on a thorough ophthalmic examination and systemic evaluation. A stepwise, multidisciplinary approach is often required.
Ocular Examination
- Slit-lamp biomicroscopy
- Intraocular pressure measurement
- Dilated fundus examination
- Optical coherence tomography (OCT)
- Fluorescein angiography
Laboratory and Imaging Tests
- Blood Tests: CBC, ESR, CRP, HLA-B27, ANA, ACE, syphilis serology
- Infectious Workup: PPD, Quantiferon, toxoplasma antibodies
- Chest Imaging: Chest X-ray or CT for sarcoidosis and TB
- MRI Brain/Spine: If neurological involvement is suspected
- Aqueous/Vitreous Tap: PCR for infectious agents in atypical cases
Uveitis Treatment Strategies
Treatment is dictated by the cause, severity, and site of inflammation. The goals are to eliminate inflammation, prevent vision loss, and treat underlying systemic disease.
Corticosteroids
- Topical steroids: Mainstay for anterior uveitis
- Periocular/intravitreal injections: For intermediate or posterior involvement
- Systemic steroids: For severe or bilateral disease
Immunosuppressive Therapy
- Steroid-sparing agents: Methotrexate, azathioprine, mycophenolate mofetil
- Biologic agents: Anti-TNF (infliximab, adalimumab) for refractory or systemic-associated uveitis
Antimicrobial Therapy
Infectious uveitis requires targeted antibiotics, antivirals, or antiparasitic agents based on the identified pathogen.
Surgical Interventions
- Vitrectomy: For diagnostic purposes or management of complications
- Cataract surgery: In cases of steroid-induced cataracts, performed under controlled inflammation
Complications of Untreated or Recurrent Uveitis
Delayed or inadequate treatment may result in irreversible vision-threatening complications:
- Cataract formation
- Glaucoma
- Cystoid macular edema
- Retinal detachment
- Optic nerve damage
- Choroidal neovascularization
Long-Term Management and Follow-Up
Uveitis often requires prolonged monitoring and treatment to prevent recurrence. A coordinated approach between ophthalmologists and rheumatologists or infectious disease specialists is essential.
Key Components of Ongoing Care:
- Regular ophthalmic exams to monitor inflammation and ocular pressure
- Tapering steroids under supervision
- Monitoring for systemic side effects of immunosuppressive drugs
- Patient education on symptom awareness and medication adherence
Frequently Asked Questions:
What is the most common type of uveitis?
Anterior uveitis is the most prevalent form, accounting for 60–90% of all cases.
Can uveitis be cured?
While some cases are self-limiting or fully responsive to treatment, others require lifelong management to prevent recurrence.
Is uveitis a sign of a systemic disease?
Yes, it can be associated with autoimmune or infectious systemic diseases, warranting comprehensive evaluation.
How is uveitis different from conjunctivitis?
Unlike conjunctivitis, uveitis typically causes deeper eye pain, photophobia, and can threaten vision if untreated.
Can stress trigger uveitis?
Stress alone is not a direct cause but may exacerbate autoimmune conditions that trigger uveitis.