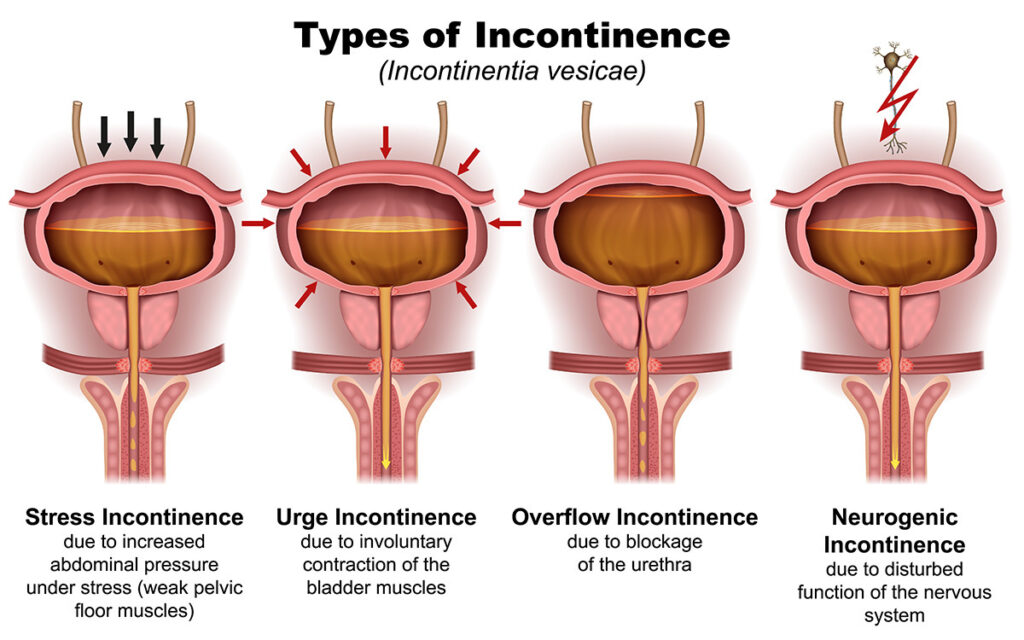
Urinary urge incontinence is the involuntary leakage of urine associated with a sudden and intense urge to urinate. It is a symptom of overactive bladder (OAB) and affects millions worldwide, particularly older adults and women. Unlike stress incontinence, which occurs due to physical pressure on the bladder (e.g., coughing or sneezing), urge incontinence arises from involuntary detrusor muscle contractions that cause an uncontrollable need to void.
Urge incontinence can severely impact daily functioning, emotional well-being, and social confidence. Identifying the correct etiology and employing individualized treatment is key to restoring quality of life.
Recognizing the Symptoms of Urinary Urge Incontinence
Urge incontinence is typically part of the overactive bladder syndrome. The hallmark symptoms include:
- Sudden, intense urge to urinate
- Involuntary urine leakage before reaching the toilet
- Increased urinary frequency (more than 8 times per day)
- Nocturia (waking two or more times at night to urinate)
- Feeling of incomplete bladder emptying
In some individuals, these symptoms may coexist with stress incontinence, resulting in mixed urinary incontinence.
Anatomy of the Lower Urinary Tract and Urge Incontinence Pathway
To understand urge incontinence, one must comprehend the normal micturition process and where dysfunction occurs.
Diagram: Normal vs. Overactive Bladder Function
Overactive detrusor activity is central to the mechanism of urinary urge incontinence.
Major Causes and Risk Factors of Urinary Urge Incontinence
Urinary urge incontinence results from neurogenic or myogenic dysfunction affecting bladder control mechanisms.
1. Neurological Causes
- Stroke
- Multiple sclerosis (MS)
- Parkinson’s disease
- Spinal cord injuries
- Diabetic neuropathy
These conditions interfere with the brain-bladder communication, leading to uninhibited contractions.
2. Non-Neurological Causes
- Urinary tract infections
- Bladder stones or tumors
- Bladder inflammation (cystitis)
- Excessive caffeine, alcohol, or fluid intake
- Medications (e.g., diuretics, sedatives)
3. Age and Hormonal Changes
- Estrogen deficiency in postmenopausal women may weaken urethral closure mechanisms.
- Aging leads to reduced bladder capacity and detrusor instability.
4. Other Contributing Factors
- Obesity
- Chronic constipation
- Pelvic surgeries
- Pelvic organ prolapse
Diagnosing Urge Incontinence: Clinical and Investigative Approach
Timely and precise diagnosis is essential to identify treatable causes and tailor therapy.
Medical History
- Onset, frequency, and severity of symptoms
- Triggers (e.g., hearing running water, anxiety)
- Fluid intake patterns
- Bowel habits and obstetric history
Physical Examination
- Abdominal and pelvic examination
- Neurological assessment
- Pelvic organ prolapse evaluation in women
- Prostate evaluation in men
Diagnostic Tests
- Urinalysis: To exclude infection or hematuria
- Postvoid residual (PVR) measurement: Assesses incomplete emptying
- Bladder diary: Tracks frequency, volume, leakage episodes
- Urodynamic studies: Confirms detrusor overactivity
- Cystoscopy: Excludes bladder lesions in refractory cases
Comprehensive Treatment Options for Urinary Urge Incontinence
1. Behavioral and Lifestyle Modifications
- Bladder Training: Gradually increasing intervals between voiding
- Scheduled Voiding: Preventing urgency by timed urination
- Fluid Management: Reducing evening fluid intake, limiting bladder irritants
- Weight Loss: Proven to reduce incontinence episodes
- Pelvic Floor Muscle Training (PFMT): Strengthens urethral support structures
2. Pharmacological Therapy
Medications target detrusor muscle activity and include:
- Antimuscarinics: Oxybutynin, tolterodine, solifenacin
- Reduce bladder contractions
- Side effects: dry mouth, constipation, blurred vision
- Beta-3 Agonists: Mirabegron
- Promote bladder relaxation with fewer side effects
- Suitable alternative for elderly or those intolerant to antimuscarinics
- Topical Estrogen (Women): Improves urethral vascularization in postmenopausal women
3. Minimally Invasive Procedures
- Botulinum Toxin A (Botox) Injections: Administered into the bladder wall to relax the detrusor muscle
- Temporary relief lasting 6–12 months
- Requires intermittent catheterization in some cases
- Peripheral Tibial Nerve Stimulation (PTNS): Neuromodulation therapy using electrical stimulation of tibial nerve
- Sacral Neuromodulation (InterStim): Implanted device modulates sacral nerves controlling bladder function
4. Surgical Interventions
Rarely required but considered for severe refractory cases:
- Bladder augmentation (augmentation cystoplasty)
- Urinary diversion procedures
Managing Urge Incontinence in Special Populations
In Elderly Patients
- Emphasis on non-pharmacological therapies to minimize polypharmacy
- Frequent monitoring for cognitive or mobility limitations
In Men with Benign Prostatic Hyperplasia (BPH)
- Combined treatment targeting prostate enlargement and bladder overactivity
- Caution with anticholinergics due to potential urinary retention
Preventive Measures for Long-Term Bladder Health
- Limit bladder irritants (caffeine, carbonated drinks, alcohol)
- Maintain healthy weight
- Avoid constipation with dietary fiber
- Practice pelvic floor exercises regularly
- Stay physically active to improve bladder control and coordination
Frequently Asked Questions:
Q1. Is urinary urge incontinence the same as overactive bladder?
Urinary urge incontinence is a symptom of overactive bladder, but not all OAB patients experience leakage.
Q2. Can urge incontinence be cured?
While not always curable, it is highly manageable through a combination of lifestyle, medications, and therapy.
Q3. How effective is bladder training?
Bladder training can reduce urgency episodes by 50–75% when consistently practiced for several weeks.
Q4. What foods or drinks should I avoid with urge incontinence?
Avoid caffeine, alcohol, artificial sweeteners, spicy foods, citrus fruits, and carbonated beverages.
Q5. Are medications safe long-term for treating urge incontinence?
Most are well tolerated with monitoring. Some may require dose adjustments due to side effects or comorbidities.
Urinary urge incontinence, though common and often distressing, is a treatable condition. A structured approach combining lifestyle adjustments, pharmacotherapy, and advanced interventions enables significant symptom relief and improved quality of life. Early diagnosis and individualized care remain the cornerstone of effective bladder control management.