Uremic bleeding tendency is a well-recognized hemorrhagic disorder observed in patients with advanced chronic kidney disease (CKD) or end-stage renal disease (ESRD). It is primarily attributed to qualitative platelet dysfunction, with normal platelet counts yet significantly impaired platelet adhesion and aggregation. Understanding the multifactorial pathophysiology and clinical implications of this condition is critical to prevent and manage life-threatening hemorrhagic episodes in uremic patients.
Pathophysiology of Uremic Bleeding: Disruption of Hemostasis in CKD
The uremic milieu disrupts normal hemostatic mechanisms, affecting the vascular endothelium, platelet function, and coagulation factors. The bleeding tendency in uremia is primarily due to platelet dysfunction, despite normal coagulation profiles and platelet counts.
Key Pathophysiological Mechanisms:
- Defective Platelet Adhesion and Aggregation
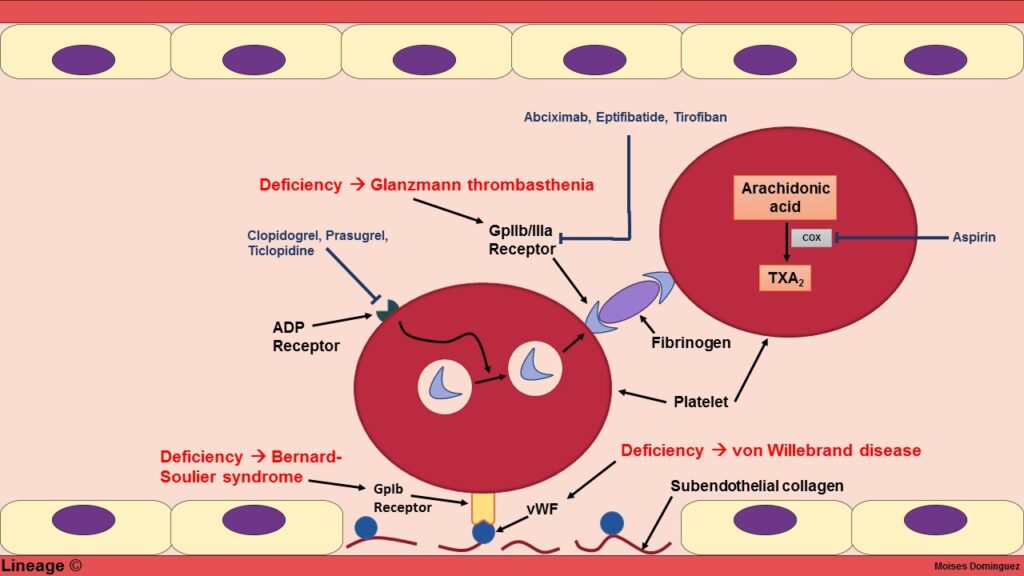
Uremic toxins such as guanidinosuccinic acid inhibit platelet function. There is also reduced glycoprotein IIb/IIIa receptor activity and decreased thromboxane A2 synthesis. - Abnormal von Willebrand Factor (vWF) Function
vWF levels may be elevated, but its function is impaired in uremia, contributing to suboptimal platelet adhesion to the subendothelium. - Anemia-Induced Hemostatic Imbalance
Decreased red cell mass leads to reduced platelet margination and impaired contact with the endothelium, worsening bleeding tendency. - Nitric Oxide (NO) Overproduction
Elevated NO levels in uremia inhibit platelet activation and vascular constriction, promoting bleeding. - Endothelial Dysfunction and Capillary Fragility
Inflammation, oxidative stress, and toxin accumulation damage the vascular lining, increasing bleeding risk.
Clinical Features of Uremic Bleeding Tendency
The bleeding profile in uremic patients ranges from mild to severe. It often presents with mucocutaneous manifestations but can escalate to life-threatening hemorrhage.
Common Clinical Presentations:
- Easy bruising and purpura
- Epistaxis (nosebleeds)
- Gingival bleeding
- Gastrointestinal bleeding (melena, hematemesis)
- Menorrhagia
- Prolonged bleeding after minor injuries or surgical procedures
- Rarely, intracranial or retroperitoneal hemorrhages
Unlike classical coagulopathies, bleeding in uremia is more often superficial and mucosal rather than deep tissue or joint-related.
Diagnostic Evaluation: Assessing Bleeding in Uremic Patients
The evaluation of uremic bleeding focuses on functional assays, as standard coagulation tests often remain normal.
Key Laboratory Findings:
| Test | Result in Uremia |
|---|---|
| Platelet Count | Normal |
| Bleeding Time | Prolonged |
| Prothrombin Time (PT) | Normal |
| Activated Partial Thromboplastin Time (aPTT) | Normal |
| Platelet Aggregometry | Abnormal responses to collagen, ADP, epinephrine |
| vWF Antigen | Elevated or normal |
| Hemoglobin | Frequently low due to anemia |
Bleeding time remains a traditional though less commonly used test due to its variability. Modern diagnostic strategies increasingly rely on platelet function assays and thromboelastography (TEG).
Management of Uremic Bleeding Tendency: Evidence-Based Interventions
Effective treatment of uremic bleeding involves correction of platelet dysfunction and mitigating risk factors. Individualized management based on clinical severity and procedural needs is essential.
Core Treatment Strategies:
1. Dialysis Optimization
- Regular and intensified dialysis helps reduce circulating uremic toxins.
- Hemodialysis improves platelet function significantly within days.
2. Desmopressin (DDAVP)
- Promotes release of vWF and factor VIII
- Dose: 0.3 mcg/kg IV over 20–30 minutes; effect lasts 4–8 hours
- Used preoperatively or for acute bleeding control
3. Cryoprecipitate
- Contains fibrinogen, vWF, and factor VIII
- Used in acute severe bleeding episodes
4. Estrogen Therapy
- Oral or IV conjugated estrogens shown to improve platelet function over 5–7 days
- Especially useful in patients refractory to DDAVP
5. Correcting Anemia
- Maintain hemoglobin ≥10 g/dL with erythropoiesis-stimulating agents (ESAs)
- Red cell transfusions in acute hemorrhage
6. Platelet Transfusion
- Reserved for thrombocytopenia or platelet count <50,000/mm³ during major bleeding or surgery
7. Avoidance of Antiplatelet Agents
- NSAIDs and aspirin worsen bleeding risk
- Use cautiously and discontinue preoperatively
Uremic Bleeding in Surgical and Interventional Settings
Patients with uremic bleeding tendencies undergoing surgical or invasive procedures require careful hemostatic preparation.
Preoperative Recommendations:
- Hemodialysis within 24 hours pre-surgery
- DDAVP or cryoprecipitate administration prior to procedure
- Maintain hemoglobin ≥10 g/dL
- Minimize use of anticoagulants and avoid unnecessary vascular trauma
Uremic Bleeding vs. Other Hemorrhagic Disorders
| Feature | Uremic Bleeding | Hemophilia | Thrombocytopenia | vWD |
|---|---|---|---|---|
| Platelet Count | Normal | Normal | Low | Normal |
| Bleeding Site | Mucosal | Joints, muscles | Skin, mucosa | Mucosa |
| Bleeding Time | Prolonged | Normal | Prolonged | Prolonged |
| PT/aPTT | Normal | ↑ aPTT | Normal | Normal or ↑ aPTT |
| Response to DDAVP | Good | Variable | Poor | Good (in Type 1) |
Prognosis and Long-Term Outlook
With optimized dialysis and hemostatic control, uremic bleeding tendency can be effectively managed. However, recurrent bleeding episodes may impair quality of life and increase hospitalization rates.
Prognostic Indicators:
- Effective dialysis regimen
- Adequate anemia correction
- Absence of concomitant anticoagulant use
- Early intervention before surgery or invasive procedures
Uremic bleeding tendency remains a significant clinical concern in patients with CKD and ESRD. Driven by complex platelet dysfunction and vascular abnormalities, it requires precise diagnostic assessment and tailored therapeutic strategies. Through rigorous dialysis, pharmacologic interventions such as desmopressin and estrogens, and meticulous perioperative care, clinicians can significantly reduce bleeding risk and improve outcomes in this vulnerable population.