Ureaplasma pneumonia represents an uncommon yet clinically significant respiratory infection primarily caused by Ureaplasma urealyticum or Ureaplasma parvum. These organisms, members of the Mycoplasmataceae family, are atypical bacteria that lack a cell wall, leading to unique diagnostic and therapeutic challenges. Though commonly colonizing the urogenital tract, Ureaplasma species can invade the lower respiratory tract, particularly in immunocompromised hosts, neonates, and patients with chronic pulmonary disorders.
Pathogenesis of Ureaplasma Respiratory Infection
Ureaplasma species act as opportunistic pathogens. In susceptible individuals, colonization of the respiratory mucosa leads to inflammation, tissue damage, and atypical pneumonia. Unlike typical bacterial pneumonia, Ureaplasma-induced infections do not produce purulent sputum or lobar consolidation on imaging.
Epidemiology and High-Risk Populations
Ureaplasma pneumonia remains underdiagnosed due to its subtle clinical presentation and specialized diagnostic requirements. While rare in healthy individuals, the condition is notably prevalent in the following groups:
- Preterm Neonates: Often associated with bronchopulmonary dysplasia (BPD)
- Organ Transplant Recipients
- Patients with Hypogammaglobulinemia
- Individuals with HIV/AIDS
- Prolonged Mechanical Ventilation Cases
- Patients on Immunosuppressants or Chemotherapy
Clinical Features and Symptoms of Ureaplasma Pneumonia
The symptoms of ureaplasma-related pulmonary infection often mimic other causes of atypical pneumonia but may be more insidious and less responsive to empirical beta-lactam antibiotics.
Common Clinical Signs:
- Persistent dry cough
- Low-grade fever
- Dyspnea or shortness of breath
- Chest discomfort
- Hypoxia in severe cases
- Progressive respiratory failure (in neonates and immunocompromised individuals)
In neonates, signs may overlap with neonatal respiratory distress syndrome or BPD, necessitating precise microbiological confirmation.
Diagnostic Evaluation of Ureaplasma in Lungs
Due to their lack of a peptidoglycan cell wall, Ureaplasma organisms are not visible on Gram stain and cannot be cultured using standard bacterial media. Targeted diagnostics are essential.
Diagnostic Modalities:
- Polymerase Chain Reaction (PCR): High sensitivity and specificity for Ureaplasma urealyticum and Ureaplasma parvum
- Culture in Specialized Media: Requires urea-containing broth and enriched CO₂ environments
- Bronchoalveolar Lavage (BAL): Useful in ventilated or critically ill patients
- Next-Generation Sequencing (NGS): Detects Ureaplasma in polymicrobial settings
- Serology: Limited utility due to cross-reactivity and delayed response
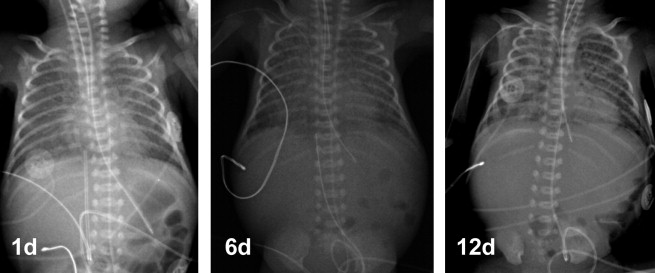
Radiographic Findings
Unlike bacterial pneumonia, Ureaplasma pneumonia shows non-specific findings on imaging. Chest radiographs or CT scans may reveal:
- Interstitial infiltrates
- Ground-glass opacities
- Patchy bilateral consolidations
- Absence of pleural effusion or cavitations
These findings often overlap with viral or mycoplasma pneumonia, reinforcing the need for microbial testing.
Treatment of Ureaplasma-Induced Pneumonia
Due to their intrinsic resistance to beta-lactam antibiotics, treatment of Ureaplasma infections relies on antibiotics that target ribosomal protein synthesis or DNA replication.
First-Line Agents:
- Macrolides (Azithromycin, Clarithromycin): Preferred due to intracellular activity
- Fluoroquinolones (Levofloxacin, Moxifloxacin): Effective in adults; limited use in pediatrics
- Tetracyclines (Doxycycline): Effective in non-pregnant adults and older children
Duration: 7–14 days, depending on severity and immune status
Note: Resistance to macrolides and tetracyclines has been reported; susceptibility testing should guide therapy when available.
Complications of Untreated Ureaplasma Pneumonia
Unaddressed or improperly treated Ureaplasma pneumonia can lead to several adverse outcomes, especially in vulnerable populations.
Potential Complications:
- Acute Respiratory Distress Syndrome (ARDS)
- Chronic Lung Disease in Neonates (e.g., BPD)
- Sepsis and Multi-organ Dysfunction
- Empirical Antibiotic Resistance
- Prolonged ICU Stay and Ventilator Dependence
Preventive Strategies and Infection Control
Prevention of Ureaplasma pneumonia is largely supportive and focused on minimizing exposure in high-risk settings.
Key Measures:
- Strict NICU Protocols: Reduce transmission in neonatal units
- Screening in Immunocompromised Hosts: Especially before organ transplantation
- Judicious Use of Broad-Spectrum Antibiotics: Avoid disruption of normal flora
- Prophylactic Macrolides: Considered in certain transplant protocols
Currently, no vaccine exists for Ureaplasma species.
Comparative Insight: Ureaplasma vs. Other Atypical Pneumonias
| Feature | Ureaplasma Pneumonia | Mycoplasma Pneumonia | Chlamydophila Pneumonia |
|---|---|---|---|
| Causative Organism | Ureaplasma urealyticum | Mycoplasma pneumoniae | Chlamydophila pneumoniae |
| Gram Stain | Not visible | Not visible | Gram-negative (weak) |
| Cell Wall | Absent | Absent | Present |
| Common in | Neonates, immunocompromised | School-aged children, adults | Elderly |
| Response to Beta-lactams | Ineffective | Ineffective | Limited |
| Diagnostic Tool | PCR, culture | PCR, serology | PCR, serology |
Ureaplasma pneumonia, though less commonly identified, poses significant risks in specific populations such as neonates and immunocompromised adults. Early recognition through advanced diagnostics and targeted therapy is essential for effective management. Unlike typical pneumonias, Ureaplasma infections require awareness of their atypical presentation, unique resistance patterns, and need for specialized treatment regimens. With the growing use of molecular diagnostics, accurate identification and tailored care are now achievable, minimizing complications and improving outcomes.