Haemophilus influenzae is a significant bacterial pathogen associated with upper respiratory tract infections (URTIs), particularly in children and immunocompromised individuals. While viral agents account for most URTIs, bacterial infections caused by H. influenzae are notable for their potential to progress rapidly and cause complications. Understanding the mechanisms, clinical presentation, diagnostic approach, and therapeutic options is essential for prompt and effective management.
Understanding Haemophilus influenzae: Overview and Classification
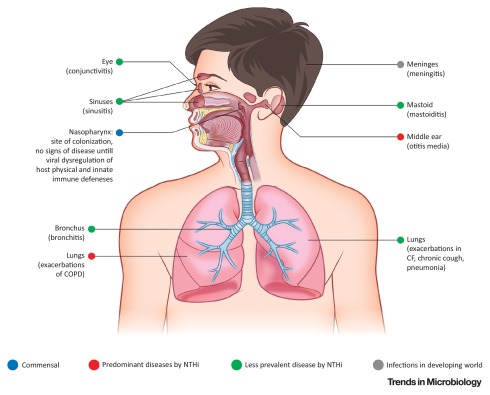
Haemophilus influenzae is a Gram-negative, coccobacillary bacterium classified into typeable and non-typeable strains:
- Typeable strains (e.g., Hib – type b): Encapsulated and more virulent; responsible for invasive diseases.
- Non-typeable strains (NTHi): Lack a polysaccharide capsule; commonly colonize the nasopharynx and are implicated in localized respiratory infections.
Primary Infections Caused by H. influenzae
- Sinusitis
- Otitis media
- Epiglottitis
- Pharyngitis
- Tracheobronchitis
- Rarely, pneumonia and sepsis
Transmission and Pathogenesis of H. influenzae-Associated URTI
Transmission occurs via respiratory droplets from an infected or asymptomatic carrier. Once inhaled, H. influenzae adheres to the mucosal epithelium of the nasopharynx and upper airway using pili and surface adhesins.
The bacterium produces IgA protease, which degrades host immunoglobulin A and facilitates colonization. In typeable strains, the capsule impedes phagocytosis and complement-mediated lysis, enhancing pathogenicity.
Clinical Features of Upper Respiratory Infection Due to Haemophilus influenzae
Common Symptoms
| Symptom | Description |
|---|---|
| Sore throat | Mucosal inflammation of the pharynx |
| Nasal congestion | Due to mucosal swelling and purulent discharge |
| Cough | Often productive, may persist several weeks |
| Low-grade fever | More common in localized infections |
| Ear pain | Involvement of middle ear in otitis media |
| Stridor or dyspnea | Indicative of laryngeal or epiglottic involvement |
Severe Manifestations
- Epiglottitis: Life-threatening; characterized by drooling, difficulty breathing, and muffled voice.
- Sinusitis: Persistent facial pain, pressure, and fever.
- Tracheitis: Barking cough and airway obstruction.
Risk Factors and Vulnerable Populations
- Infants and toddlers (especially <5 years)
- Unvaccinated individuals (against Hib)
- Patients with COPD or asthma
- Smokers
- Immunocompromised patients (e.g., HIV, chemotherapy)
- Elderly individuals
Diagnostic Evaluation and Microbiological Identification
Clinical Diagnosis
- Based on history, physical examination, and symptom profile
- In cases with severe or persistent symptoms, further testing is warranted
Laboratory Investigations
- Throat swab culture: Identifies H. influenzae, especially in cases of pharyngitis or epiglottitis
- Nasopharyngeal swab PCR: Highly sensitive and specific
- Blood culture: Required for suspected systemic infection
- Imaging (X-ray or CT scan): For sinusitis or epiglottitis
- Lateral neck radiograph: “Thumb sign” in epiglottitis
Treatment Strategies for H. influenzae Upper Respiratory Infection
Empiric and Targeted Antibiotic Therapy
Antibiotic selection depends on local resistance patterns and clinical severity.
| Antibiotic | Indications |
|---|---|
| Amoxicillin-clavulanate | First-line for non-severe cases |
| Cefuroxime | Second-generation cephalosporin |
| Ceftriaxone/Cefotaxime | For severe or systemic infections |
| Azithromycin/Clarithromycin | Alternative in penicillin allergy |
Note: Many strains produce β-lactamase and are resistant to ampicillin; hence β-lactamase inhibitors are essential.
Supportive Measures
- Analgesics (e.g., ibuprofen or acetaminophen)
- Hydration
- Humidified air for airway comfort
- Antipyretics for fever
Hospitalization Criteria
- Suspected epiglottitis
- Signs of airway obstruction
- Severe systemic symptoms
- Infants or immunocompromised individuals
Prevention and Vaccination
Hib Vaccine
The Haemophilus influenzae type b (Hib) conjugate vaccine is a critical tool in preventing severe infections.
- Routine pediatric vaccination schedule: 2, 4, 6, and 12–15 months
- Catch-up vaccination for unvaccinated children <5 years
- High-risk adult groups (e.g., asplenia, bone marrow transplant recipients)
Infection Control Measures
- Hand hygiene
- Cough etiquette
- Avoiding contact with infected individuals
- Chemoprophylaxis for close contacts in invasive Hib disease (Rifampin)
Complications of Untreated H. influenzae Upper Respiratory Infection
- Meningitis (in children, if bacteremia develops)
- Sepsis
- Otitis media with effusion
- Obstructive epiglottitis
- Chronic sinusitis
Early intervention with appropriate antibiotics can prevent these outcomes.
Prognosis and Recovery Outlook
When identified and treated early, Haemophilus influenzae URIs generally resolve without long-term effects. In high-risk or unvaccinated individuals, delayed treatment may lead to invasive complications, emphasizing the importance of prompt clinical evaluation.
Upper respiratory tract infections due to Haemophilus influenzae present a substantial health concern, especially in vulnerable populations. Clinicians must maintain a high index of suspicion for bacterial involvement in severe or persistent URTI cases. The integration of vaccination, timely diagnosis, and targeted therapy remains the cornerstone of effective management and complication prevention.