Upper respiratory infection (URI), also known as an upper respiratory tract infection, encompasses a group of illnesses affecting the nose, sinuses, pharynx, and larynx. URIs are among the most frequent reasons for healthcare visits globally, significantly impacting productivity and quality of life. A clear understanding of the etiology, clinical manifestations, treatment options, and preventive measures is essential for effective management and control of this highly prevalent condition.

Overview of Upper Respiratory Infection
Upper respiratory infections are primarily viral in origin and are transmitted through airborne droplets, direct contact, or contaminated surfaces. The most common types include:
- Common Cold (Rhinovirus)
- Pharyngitis (often caused by adenoviruses or streptococcus)
- Laryngitis
- Sinusitis
- Epiglottitis (less common but potentially severe)
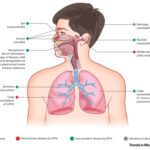
Affected Anatomical Structures
URI targets the upper airway, which includes:
- Nasal cavity
- Paranasal sinuses
- Pharynx
- Larynx
Pathogenesis of Upper Respiratory Tract Infections
URIs result from the invasion of pathogens—primarily viruses—into the mucosal lining of the upper respiratory tract. The infection triggers an inflammatory response, leading to symptoms like congestion, coughing, and throat irritation.
Causes and Common Pathogens
Viral Causes (90–95% of cases)
- Rhinovirus – Most prevalent, especially in fall and spring
- Coronavirus – Including seasonal types
- Adenovirus
- Parainfluenza virus
- Respiratory syncytial virus (RSV)
- Influenza virus
Bacterial Causes (5–10%)
Though rare, some cases involve secondary bacterial infections:
- Streptococcus pyogenes (group A strep) – Pharyngitis
- Haemophilus influenzae – Sinusitis, otitis media
- Streptococcus pneumoniae
- Moraxella catarrhalis
Risk Factors for URI
- Close contact with infected individuals
- Cold weather or seasonal changes
- Poor ventilation in indoor spaces
- Weakened immune system
- Smoking and air pollutants
- Chronic respiratory conditions like asthma
Signs and Symptoms of Upper Respiratory Infection
Symptoms may vary depending on the specific area affected, but common features include:
| Symptom | Description |
|---|---|
| Nasal congestion | Blocked or runny nose due to mucus overproduction |
| Sore throat | Pain, scratchiness, or irritation in the pharynx |
| Sneezing | Reflex response to nasal irritation |
| Cough | Often dry initially, may become productive |
| Headache | Resulting from sinus pressure or inflammation |
| Fever | Low-grade in viral cases, high in bacterial infections |
| Fatigue | Generalized malaise and tiredness |
Red Flag Symptoms (indicating complications)
- Difficulty breathing
- Persistent high fever (>102°F)
- Severe sore throat with drooling (epiglottitis)
- Neck stiffness
- Chest pain
Diagnostic Evaluation
Clinical Diagnosis
Most URIs are diagnosed based on history and physical examination. Specific tests are reserved for severe or persistent cases.
Diagnostic Tests
- Rapid strep test – For suspected streptococcal pharyngitis
- Throat culture – Confirms bacterial cause
- PCR-based respiratory panel – Detects viral pathogens
- Imaging (CT/X-ray) – For suspected sinusitis complications
Treatment Options for URI
Symptomatic Relief for Viral URIs
- Analgesics (Acetaminophen or Ibuprofen) – Reduce fever and pain
- Decongestants (Pseudoephedrine, Oxymetazoline) – Relieve nasal blockage
- Antihistamines (Diphenhydramine, Loratadine) – Control sneezing and runny nose
- Cough suppressants (Dextromethorphan) – For dry, non-productive cough
- Expectorants (Guaifenesin) – Loosen mucus in productive cough
- Saline nasal sprays or steam inhalation – Moisturize airways and improve breathing
Antibiotics for Bacterial Infections
Only used when bacterial infection is confirmed or strongly suspected:
- Penicillin or Amoxicillin – First-line for streptococcal pharyngitis
- Amoxicillin-clavulanate or Doxycycline – For sinusitis
Inappropriate antibiotic use contributes to antimicrobial resistance and should be avoided in viral infections.
Prevention Strategies for Upper Respiratory Infections
Personal Hygiene
- Frequent handwashing with soap for at least 20 seconds
- Use of alcohol-based hand sanitizers when soap is unavailable
- Avoid touching the face, especially nose and mouth
Respiratory Etiquette
- Cover nose and mouth while sneezing or coughing
- Dispose of tissues properly
- Use of face masks in crowded or enclosed spaces
Lifestyle Measures
- Adequate sleep and hydration
- Nutrient-rich diet to support immunity
- Regular exercise to enhance respiratory function
Vaccination
- Influenza vaccine – Annual protection against seasonal flu
- COVID-19 vaccine – Prevents SARS-CoV-2 infection
- Pneumococcal vaccine – For high-risk populations
Complications of Untreated or Severe URIs
- Secondary bacterial infection
- Acute sinusitis or otitis media
- Bronchitis or pneumonia
- Exacerbation of asthma or COPD
- Rare but serious: peritonsillar abscess, epiglottitis
Prognosis and Recovery Timeline
- Most URIs resolve within 7 to 10 days
- Cough may persist up to 3 weeks post-infection
- Prompt symptom management and supportive care accelerate recovery
Upper respiratory infections are among the most common and contagious illnesses affecting people of all ages. Timely recognition, appropriate management, and preventive practices are crucial for minimizing spread and ensuring faster recovery. By understanding the underlying causes and differentiating between viral and bacterial infections, we can significantly improve patient outcomes while reducing unnecessary medication use.