Uncinariasis, commonly known as hookworm infection, is a parasitic disease caused primarily by species of the genus Ancylostoma and Necator. It remains a significant public health concern in tropical and subtropical regions, where poor sanitation facilitates transmission. This comprehensive article delineates the epidemiology, pathophysiology, clinical manifestations, diagnostic protocols, treatment regimens, and preventive strategies related to uncinariasis, providing a resource grounded in scientific rigor and clinical relevance.
Uncinariasis Overview: Etiology and Epidemiological Insights
Uncinariasis is caused by the intestinal nematode parasites Ancylostoma duodenale and Necator americanus. These hookworms inhabit the small intestine, where they attach to the mucosa and feed on the host’s blood, leading to chronic blood loss and subsequent iron-deficiency anemia.
Global Prevalence and Risk Factors
The disease predominantly affects impoverished communities with inadequate sanitation and hygiene infrastructure. It is endemic in regions of Sub-Saharan Africa, Southeast Asia, Latin America, and parts of the southern United States. Transmission correlates strongly with climatic conditions that favor larval survival in warm, moist soil.
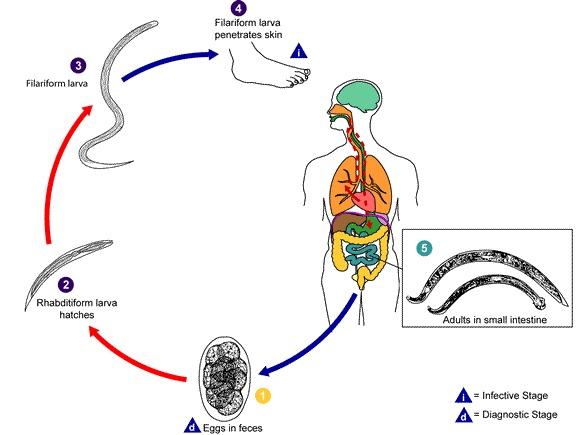
Lifecycle and Transmission Dynamics of Uncinaria
The lifecycle of Ancylostoma and Necator is a critical aspect of understanding uncinariasis transmission and control.
Upon skin penetration, larvae migrate through the bloodstream to the lungs, ascend the respiratory tract, and are swallowed into the gastrointestinal tract, where adult worms mature and reproduce.
Clinical Manifestations: Symptoms and Signs of Uncinariasis
The clinical spectrum of uncinariasis varies from asymptomatic infection to severe morbidity.
Acute Phase (Cutaneous and Pulmonary)
- Ground itch: Pruritic, erythematous rash at the site of larval penetration.
- Pulmonary symptoms: Cough, wheezing, and transient pneumonitis may develop during larval migration.
Chronic Phase (Intestinal Infection)
- Gastrointestinal symptoms: Abdominal pain, diarrhea, and anorexia.
- Iron-deficiency anemia: Due to chronic blood loss caused by adult worms feeding on intestinal mucosa.
- Protein malnutrition: Resulting from chronic intestinal blood loss.
- Growth retardation: Particularly in children due to nutritional deficiencies.
Diagnostic Strategies for Accurate Detection of Uncinariasis
Diagnosis relies on a combination of clinical suspicion and laboratory testing.
- Stool microscopy: Identification of characteristic hookworm eggs via direct smear or concentration techniques remains the gold standard.
- Complete blood count: Reveals anemia, eosinophilia, and occasionally leukocytosis.
- Serological assays: Useful in non-endemic settings or in early infections before egg shedding.
Treatment Protocols: Pharmacological Management of Uncinariasis
Effective treatment is essential to reduce morbidity and interrupt transmission cycles.
First-Line Anthelmintics
- Albendazole: 400 mg single dose is widely effective with a favorable safety profile.
- Mebendazole: Administered as 100 mg twice daily for three days.
- Pyrantel pamoate: Alternative agent with comparable efficacy.
Supportive Care
- Iron supplementation: Critical for correcting anemia.
- Nutritional support: Addresses protein and micronutrient deficiencies.
Preventive Measures and Public Health Interventions
Preventing uncinariasis requires a multifaceted approach:
- Improved sanitation: Construction and maintenance of latrines to reduce soil contamination.
- Health education: Promoting footwear use and hygienic practices.
- Mass drug administration: Periodic anthelmintic distribution in endemic communities.
- Environmental control: Soil management to decrease larval habitats.
Complications and Long-Term Outcomes of Untreated Uncinariasis
Without intervention, uncinariasis may result in severe anemia, leading to fatigue, developmental delays in children, and increased susceptibility to other infections. Chronic infection may exacerbate existing comorbidities, including cardiovascular and respiratory conditions.
Uncinariasis continues to impose a considerable health burden in vulnerable populations. Comprehensive understanding of its lifecycle, clinical features, and diagnostic methods facilitates timely intervention. Employing effective pharmacotherapy combined with preventive public health measures can markedly reduce the incidence and impact of this parasitic infection.