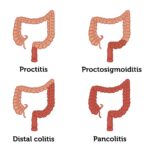
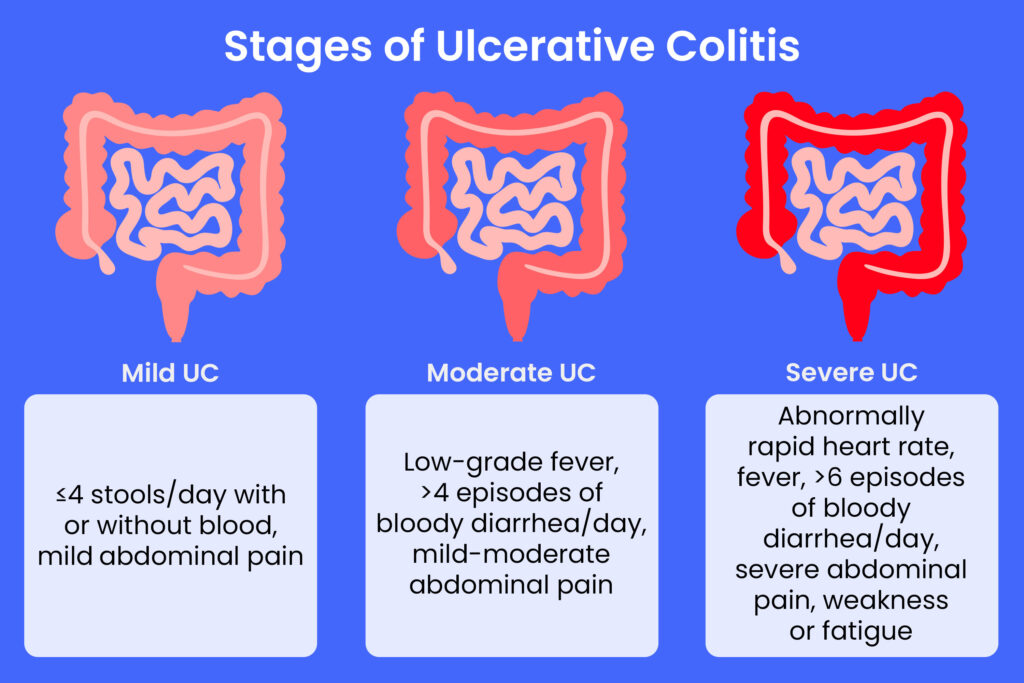
Ulcerative colitis (UC) remission signifies a critical therapeutic milestone in the management of this chronic inflammatory bowel disease. Achieving and maintaining remission not only alleviates the debilitating symptoms but also significantly reduces the risk of complications, enhances patient quality of life, and mitigates long-term health risks including colorectal cancer. This article offers an exhaustive overview of ulcerative colitis remission, highlighting evidence-based approaches to induce and sustain remission, key clinical considerations, and lifestyle modifications essential for enduring disease control.
Defining Ulcerative Colitis Remission: Clinical and Endoscopic Criteria
Remission in ulcerative colitis encompasses both symptomatic relief and objective healing of the colonic mucosa.
- Clinical remission involves the resolution of symptoms such as diarrhea, rectal bleeding, abdominal pain, and urgency.
- Endoscopic remission is characterized by the absence of visible inflammation, ulcerations, and friability on colonoscopy.
Complete remission includes histological remission, where biopsy specimens reveal no microscopic inflammation, reflecting deep mucosal healing.
Induction of Remission: Therapeutic Modalities and Protocols
Effective induction therapy aims to rapidly quell active inflammation and restore intestinal integrity.
First-Line Induction Therapies
- 5-Aminosalicylic Acid (5-ASA) agents: Mesalamine remains the cornerstone for mild to moderate UC. High-dose oral and topical formulations combined optimize mucosal contact.
- Corticosteroids: Systemic corticosteroids such as prednisone are reserved for moderate to severe flares to suppress inflammation quickly. Due to adverse effects, they are not recommended for maintenance.
Advanced Induction Options
- Biologic agents: Tumor necrosis factor-alpha (TNF-α) inhibitors (e.g., infliximab, adalimumab), anti-integrin agents (vedolizumab), and interleukin inhibitors (ustekinumab) are indicated for steroid-refractory or moderate-to-severe cases.
- Janus kinase (JAK) inhibitors: Tofacitinib offers rapid symptomatic relief in refractory disease.
Maintaining Ulcerative Colitis Remission: Long-Term Strategies
Sustained remission requires a strategic maintenance plan tailored to individual disease severity and prior treatment response.
Maintenance Medications
- 5-ASA therapy: Continual use of mesalamine reduces relapse rates and is well-tolerated.
- Immunomodulators: Azathioprine and 6-mercaptopurine provide steroid-sparing effects and are vital for patients with frequent relapses.
- Biologics and small molecules: Long-term administration of biologic agents maintains mucosal healing and prevents flares in moderate to severe UC.
Monitoring and Early Detection of Relapse
Regular clinical assessment, biomarker evaluation, and endoscopic surveillance are critical to detect subclinical inflammation and preempt relapse.
- Fecal calprotectin: Elevated levels serve as a sensitive marker for intestinal inflammation and impending flare.
- C-reactive protein (CRP): Though less specific, CRP trends assist in monitoring systemic inflammation.
- Periodic colonoscopy: Enables direct visualization of mucosal status and early intervention upon detecting disease activity.
Diet and Lifestyle Modifications for Remission Maintenance
Dietary patterns and lifestyle habits substantially influence remission duration and flare frequency.
Recommended Dietary Practices
- Balanced nutrition: Emphasize high-protein, low-residue diets during flares, transitioning to fiber-rich, anti-inflammatory foods during remission.
- Avoidance of triggers: Limit alcohol, caffeine, spicy foods, and processed foods known to exacerbate symptoms.
- Hydration and supplementation: Address vitamin D, calcium, and iron deficiencies common in UC patients.
Lifestyle Considerations
- Stress management: Psychological stress is a recognized trigger; mindfulness, cognitive behavioral therapy, and physical exercise reduce flare risk.
- Smoking cessation: Smoking cessation benefits UC patients, unlike Crohn’s disease where smoking exacerbates the condition.
Complications During Remission and Preventive Measures
Even in remission, patients must remain vigilant to potential complications:
- Colorectal cancer risk: Long-standing UC increases malignancy risk; thus, adherence to surveillance colonoscopy guidelines is imperative.
- Osteoporosis: Chronic inflammation and corticosteroid use predispose to bone density loss; proactive screening and supplementation are advised.
- Extraintestinal manifestations: Joint, skin, and ocular symptoms may persist; multidisciplinary care optimizes management.
Ulcerative Colitis Remission: Patient-Centered Approach
Achieving remission is a collaborative process involving patient education, medication adherence, and regular follow-up.
- Shared decision-making: Incorporating patient preferences and values enhances adherence and outcomes.
- Symptom tracking: Use of apps and diaries facilitates early recognition of symptom changes.
- Support networks: Participation in support groups mitigates psychological burden.
Ulcerative colitis remission embodies a complex therapeutic goal encompassing symptom resolution and mucosal healing. Meticulous application of induction and maintenance therapies combined with vigilant monitoring and lifestyle adjustments enhances long-term outcomes. By adhering to a patient-centric, evidence-based strategy, we can significantly improve remission durability and quality of life for those living with ulcerative colitis.