Tubo-ovarian abscess (TOA) is a serious complication of pelvic inflammatory disease (PID), characterized by the formation of an inflammatory mass involving the fallopian tube, ovary, and adjacent pelvic organs. Most commonly occurring in reproductive-aged women, TOA presents significant morbidity and can result in long-term reproductive and systemic complications if not managed promptly.
Pathophysiology and Causes of Tubo-Ovarian Abscess
Tubo-ovarian abscess typically results from ascending polymicrobial infections, including sexually transmitted pathogens and anaerobes, which spread from the lower genital tract to the upper reproductive organs.
Key Causative Organisms:
- Neisseria gonorrhoeae
- Chlamydia trachomatis
- Anaerobic bacteria (Bacteroides, Peptostreptococcus)
- Facultative organisms (Escherichia coli)
Predisposing Risk Factors:
- Multiple sexual partners
- History of PID
- Intrauterine device (IUD) usage
- Recent gynecologic instrumentation or surgery
- Immunosuppression
Clinical Presentation and Symptoms of TOA
Symptoms of TOA are often indistinguishable from PID, but typically more severe. Clinical suspicion must remain high in patients presenting with pelvic pain and systemic symptoms.
Common Signs and Symptoms:
- Lower abdominal or pelvic pain (often unilateral)
- Fever and chills
- Vaginal discharge (purulent or foul-smelling)
- Dyspareunia
- Menstrual irregularities
- Gastrointestinal symptoms (nausea, vomiting, anorexia)
On Physical Examination:
- Adnexal tenderness
- Cervical motion tenderness
- Palpable adnexal mass on bimanual examination
Diagnostic Evaluation of Tubo-Ovarian Abscess
Prompt diagnosis is essential to avoid rupture and sepsis. A combination of laboratory tests and imaging modalities aids in confirming TOA.
Laboratory Investigations:
- Complete Blood Count (CBC): Leukocytosis with neutrophilia
- C-reactive Protein (CRP) & ESR: Elevated inflammatory markers
- Vaginal/Cervical Swabs: To detect gonorrhea, chlamydia, and other pathogens
- Blood Cultures: In febrile patients with suspected sepsis
Imaging Techniques:
Transvaginal Ultrasound (TVUS)
- First-line imaging
- Reveals complex, thick-walled adnexal mass with internal echoes
Computed Tomography (CT) or Magnetic Resonance Imaging (MRI)
- CT scan preferred if rupture suspected
- MRI provides superior soft tissue contrast for complex cases
Differential Diagnosis of Tubo-Ovarian Abscess
TOA may mimic other gynecologic and gastrointestinal conditions, making differential diagnosis critical.
Conditions to Rule Out:
- Ectopic pregnancy
- Ovarian torsion
- Ruptured ovarian cyst
- Appendicitis
- Diverticulitis
- Endometrioma
Medical and Surgical Management of TOA
Initial Medical Management
Empiric Broad-Spectrum Antibiotics:
Should cover anaerobes, Gram-negative bacilli, and sexually transmitted organisms.
Recommended Regimens:
- IV Regimen: Cefoxitin or cefotetan + doxycycline ± metronidazole
- Alternative: Clindamycin + gentamicin
- Oral Transition: After 48–72 hours of clinical improvement
Criteria for Medical Management Alone:
- Hemodynamic stability
- Abscess <9 cm
- No signs of rupture
- Good response within 48–72 hours
Indications for Surgical Intervention
- Abscess >9 cm
- Failure to improve with antibiotics
- Suspected or confirmed rupture
- Uncertain diagnosis
- Infertility workup in complex cases
Surgical Options:
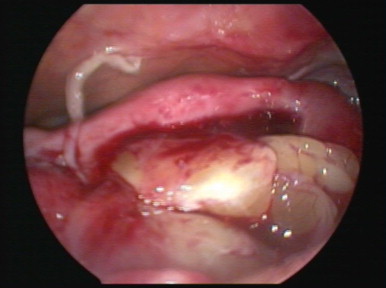
- Laparoscopy: Preferred for drainage, less invasive
- Laparotomy: For extensive disease or hemodynamic instability
- Image-Guided Percutaneous Drainage: For selected patients unfit for surgery
Complications of Untreated or Delayed TOA Management
Delayed diagnosis or inadequate treatment of TOA can result in life-threatening and fertility-threatening outcomes.
Major Complications Include:
- Abscess rupture → Peritonitis, sepsis
- Chronic pelvic pain
- Ectopic pregnancy risk
- Infertility due to tubal damage
- Adhesions and pelvic scarring
- Recurrent pelvic infections
Tubo-Ovarian Abscess in Special Populations
Adolescents
- Requires sensitive evaluation due to potential sexual abuse concerns
- Conservative antibiotic therapy preferred
Postmenopausal Women
- Rare and often associated with malignancy
- Early surgical exploration frequently indicated
Pregnancy
- Extremely rare but dangerous
- Individualized management to balance maternal and fetal safety
Prevention Strategies for TOA
Effective prevention of TOA involves early treatment of PID and STI control.
Preventive Measures:
- Prompt treatment of STIs
- Routine sexual health screening
- Consistent condom use
- Limiting the number of sexual partners
- Avoiding unnecessary gynecologic instrumentation
- Education on PID symptoms and when to seek care
Follow-Up and Long-Term Care
Patients treated for TOA require careful follow-up to ensure complete resolution and prevent recurrence.
Follow-Up Plan:
- Clinical re-evaluation within 48–72 hours of treatment initiation
- Imaging follow-up if no improvement
- Education on recurrence signs
- Fertility evaluation in selected cases
Prompt Recognition and Treatment Are Essential
Tubo-ovarian abscess represents a severe sequela of pelvic infections and demands timely recognition, accurate diagnosis, and individualized treatment. Medical therapy with broad-spectrum antibiotics remains the cornerstone for most cases, but surgical or interventional radiologic management is warranted when complications arise. With early intervention, the risks of long-term reproductive morbidity and systemic complications can be significantly reduced.

