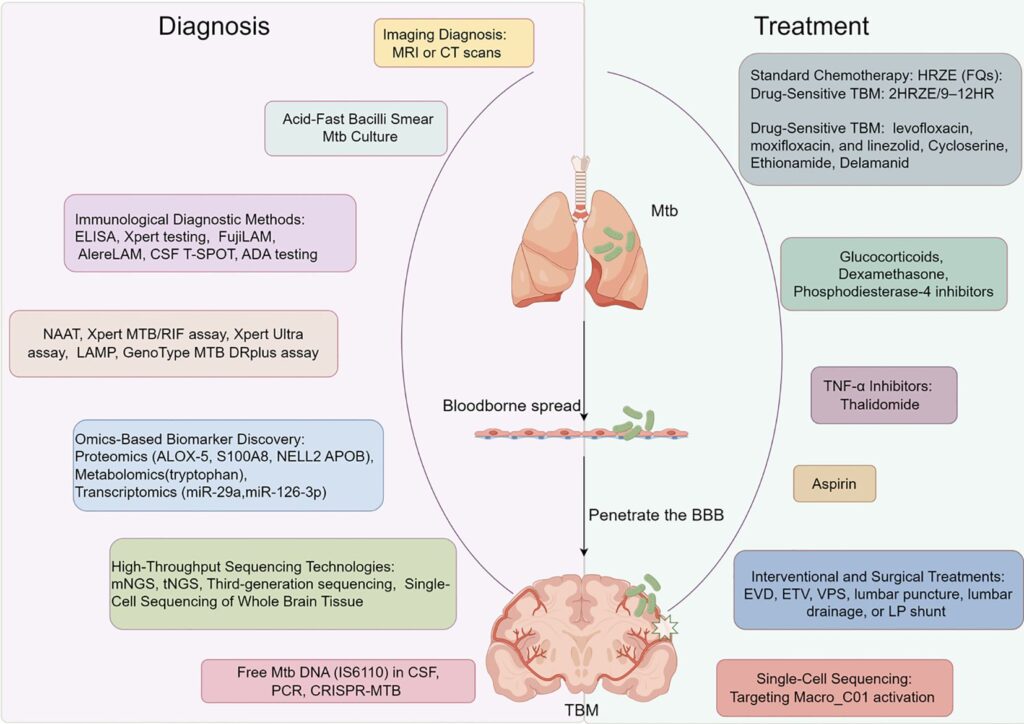
Tuberculosis meningitis (TBM) is the most severe manifestation of extrapulmonary tuberculosis, with high mortality and neurological morbidity. While standard antitubercular therapy (ATT) forms the cornerstone of treatment, adjunctive interventions are essential to modulate inflammation, reduce complications, and improve neurological outcomes.
Adjunct therapies in TBM encompass pharmacological agents such as corticosteroids, immunomodulatory treatments, and surgical management strategies. These interventions are increasingly recognized as critical in comprehensive TBM care.
Importance of Adjunctive Treatment in TBM
Adjunctive therapy addresses the intense inflammatory response within the central nervous system (CNS), which, if unchecked, leads to complications such as hydrocephalus, vasculitis, infarction, and cranial nerve palsies.
Goals of Adjunctive Therapy:
- Decrease inflammation
- Reduce cerebral edema
- Control intracranial pressure
- Prevent or mitigate neurological damage
- Enhance survival and functional recovery
Corticosteroids: Cornerstone of Adjunctive Therapy in TBM
Mechanism of Action
Corticosteroids suppress the pro-inflammatory cytokine cascade triggered by mycobacterial lysis and immune response. This limits the immune-mediated injury to the CNS.
Evidence-Based Use
Randomized controlled trials have consistently shown that adjunctive corticosteroids:
- Improve survival in HIV-negative individuals
- Reduce long-term neurological sequelae
- Are most beneficial when initiated early
Common Regimens
- Dexamethasone: IV or oral, tapered over 6–8 weeks
- Prednisolone: Alternative to dexamethasone, especially in pediatric settings
| Disease Severity | Dexamethasone Initial Dose | Duration |
|---|---|---|
| Mild | 0.3–0.4 mg/kg/day | 6 weeks taper |
| Moderate-Severe | 0.6–0.8 mg/kg/day | 6–8 weeks taper |
Immunomodulatory Adjuncts: A Growing Frontier
Although corticosteroids remain the mainstay, novel immunomodulators are being explored.
Aspirin
- Rationale: Antiplatelet and anti-inflammatory effects may reduce TBM-associated infarcts.
- Evidence: Clinical trials (e.g., LASER-TBM) have suggested modest benefits in reducing stroke incidence in TBM.
Thalidomide
- Function: Tumor necrosis factor-alpha (TNF-α) inhibitor
- Indications: Severe, steroid-refractory cases or TBM-related vasculitis
- Risks: Teratogenicity and peripheral neuropathy limit widespread use
Interferon-Gamma
- Experimental Use: Boosts macrophage activation and immune control of M. tuberculosis
- Limitations: Not routinely recommended due to cost and limited evidence
Adjunctive Management of TBM Complications
Hydrocephalus
Hydrocephalus is a common and life-threatening complication in TBM due to CSF flow obstruction from exudates.
Management:
- Medical: Acetazolamide, mannitol (temporary relief)
- Surgical:
- Ventriculoperitoneal (VP) shunt – for communicating hydrocephalus
- Endoscopic third ventriculostomy (ETV) – for non-communicating hydrocephalus
Seizures
- Management: Antiepileptic drugs (AEDs) like levetiracetam or phenytoin
- Adjunct Role: Early seizure control reduces secondary brain injury
Hyponatremia
Commonly due to:
- Syndrome of Inappropriate Antidiuretic Hormone (SIADH)
- Cerebral Salt Wasting (CSW)
Treatment varies:
- SIADH: Fluid restriction
- CSW: Sodium and volume replacement
TBM in Special Populations: Adjunctive Considerations
HIV Co-infection
Adjunctive corticosteroids in HIV-positive TBM patients remain controversial:
- Benefits in inflammation control must be weighed against the risk of opportunistic infections
- Early antiretroviral therapy (ART) can trigger Immune Reconstitution Inflammatory Syndrome (IRIS)
Pediatrics
- Greater likelihood of severe complications such as hydrocephalus
- Corticosteroids shown to reduce mortality and neurological sequelae
- Monitoring for steroid-induced side effects (e.g., growth suppression) is crucial
Adjunct Therapies in Drug-Resistant TBM
Multidrug-resistant TBM presents unique challenges where standard therapy is ineffective.
Adjunctive Measures:
- Longer and intensified ATT
- Prolonged corticosteroids
- Consideration of linezolid and fluoroquinolones
- Experimental adjuncts like host-directed therapies under investigation
Emerging Therapies and Research Directions
Ongoing research is exploring novel adjunctive interventions, including:
- Host-Directed Therapies (HDTs): Targeting immune pathways rather than bacteria
- Biomarker-driven corticosteroid dosing: Personalizing treatment based on inflammatory markers
- Anti-TNF therapies: Selective immunomodulation
- Vitamin D supplementation: Immune support and neuroprotection
Optimizing Outcomes with Adjunctive TBM Treatment
Adjunctive therapies in tuberculosis meningitis are pivotal in reducing the inflammatory burden and mitigating CNS damage. Corticosteroids remain the gold standard, supported by immunomodulators, surgical interventions, and tailored supportive care based on patient presentation. Integrating these adjuncts with early diagnosis and effective ATT forms the bedrock of modern TBM management.

