Trimetrexate, a potent dihydrofolate reductase (DHFR) inhibitor, is an antimetabolite chemotherapeutic agent primarily used in the treatment of Pneumocystis jirovecii pneumonia (PCP) in immunocompromised patients, particularly those with HIV/AIDS. It has also been explored in various cancers including colorectal carcinoma and lymphomas. Despite its therapeutic potential, trimetrexate is associated with significant toxicity risks. This article comprehensively addresses the pathophysiology, adverse effects, diagnostic considerations, and management protocols for trimetrexate toxicity.
Pharmacodynamics and Mechanism of Action
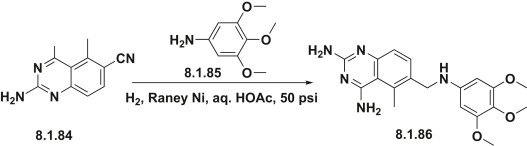
Trimetrexate is a lipophilic analog of methotrexate that inhibits DHFR, an enzyme essential for tetrahydrofolate synthesis. This inhibition disrupts DNA, RNA, and protein synthesis in rapidly dividing cells, making it effective against both neoplastic and microbial cells.
The lipophilic nature of trimetrexate facilitates cellular penetration even in the absence of folate transport mechanisms, a key distinction from methotrexate. However, this also contributes to its non-selective cytotoxicity in host tissues, especially when leucovorin rescue is inadequate.
Risk Factors for Trimetrexate Toxicity
The following conditions predispose patients to increased risk of trimetrexate-related toxicities:
- Renal or hepatic impairment
- Inadequate leucovorin rescue therapy
- High cumulative doses
- Concurrent nephrotoxic or hepatotoxic agents
- HIV/AIDS with baseline immunosuppression
- Bone marrow suppression from other therapies
Timely risk identification is essential to mitigate life-threatening complications.
Key Clinical Manifestations of Trimetrexate Toxicity
1. Myelosuppression (Hematologic Toxicity)
Trimetrexate-induced myelosuppression is dose-dependent and may be exacerbated by insufficient leucovorin rescue.
Common presentations:
- Neutropenia
- Anemia
- Thrombocytopenia
- Pancytopenia in severe cases
Consequences:
- Increased risk of infections
- Hemorrhagic complications
- Delay or discontinuation of therapy
2. Hepatotoxicity
Hepatic injury is a well-documented adverse effect, manifesting as:
- Elevated AST and ALT levels
- Hyperbilirubinemia
- Hepatic necrosis (rare but fatal)
- Jaundice
Monitoring liver enzymes during treatment is critical.
3. Gastrointestinal Toxicity
Rapidly dividing epithelial cells in the GI tract are vulnerable to trimetrexate:
- Nausea and vomiting
- Severe mucositis
- Diarrhea
- Gastrointestinal bleeding (in neutropenic patients)
4. Renal Impairment
Although less frequent than with methotrexate, trimetrexate can cause:
- Elevation in serum creatinine
- Decreased GFR
- Risk of cumulative toxicity due to impaired clearance
5. Dermatologic and Hypersensitivity Reactions
Adverse cutaneous effects may include:
- Rash
- Pruritus
- Photosensitivity
- Rare cases of Stevens-Johnson Syndrome (SJS)
6. Pulmonary Toxicity
Though uncommon, trimetrexate has been linked with:
- Interstitial pneumonitis
- Pulmonary fibrosis
These are particularly concerning in AIDS patients already vulnerable to respiratory complications.
Diagnostic Evaluation of Suspected Trimetrexate Toxicity
A systematic and timely workup is crucial. Evaluation involves clinical assessment and laboratory investigations to identify organ involvement.
Recommended Diagnostic Tests:
| Test | Purpose |
|---|---|
| CBC with differential | Assess for neutropenia, anemia, thrombocytopenia |
| LFTs (AST, ALT, bilirubin) | Detect hepatocellular injury |
| Serum creatinine, BUN | Evaluate renal function |
| Electrolyte panel | Monitor for imbalances secondary to GI loss or nephrotoxicity |
| Urinalysis | Detect nephrotoxicity |
| Chest X-ray or HRCT | In case of respiratory symptoms |
Management of Trimetrexate Toxicity
1. Immediate Discontinuation of Trimetrexate
Therapy should be suspended at the first signs of severe toxicity. The risk-to-benefit ratio must be reassessed, especially in immunocompromised patients.
2. Leucovorin (Folinic Acid) Rescue
Leucovorin is essential for counteracting the toxic effects of trimetrexate. It bypasses DHFR inhibition, replenishing folate-dependent metabolic pathways.
Protocol:
- Start 24 hours after initiating trimetrexate
- Continue for 72 hours post-final dose
- Dosage adjusted based on patient weight and serum methotrexate levels (if monitored)
3. Supportive Therapy
- Granulocyte Colony-Stimulating Factor (G-CSF):
For neutropenic patients with fever or high infection risk - Blood transfusions:
For anemia or thrombocytopenia - Antiemetics and mucosal protectants:
For gastrointestinal side effects - IV fluids and electrolyte repletion:
To manage renal and GI toxicity
4. Hepatic Support
- Monitor transaminases regularly
- Discontinue any concomitant hepatotoxic medications
- Administer hepatoprotective agents if needed (e.g., N-acetylcysteine, silymarin)
5. Renal Toxicity Management
- Hydration and avoidance of nephrotoxic agents
- Dialysis is rarely required but should be considered in severe cases of renal failure
Prevention of Trimetrexate Toxicity
Effective toxicity prevention begins with proactive measures:
- Baseline organ function assessment before therapy
- Scheduled leucovorin rescue with exact dosing protocols
- Routine monitoring of CBC, LFTs, and renal parameters
- Avoid concurrent nephrotoxic/hepatotoxic drugs
- Educate patients about early warning symptoms (fatigue, bleeding, fever, jaundice)
Trimetrexate vs. Methotrexate: Toxicity Comparison
| Feature | Trimetrexate | Methotrexate |
|---|---|---|
| Cellular entry | Passive diffusion | Active transport (RFC) |
| Nephrotoxicity | Moderate | High (especially at high doses) |
| Hepatotoxicity | Significant | Moderate to significant |
| Leucovorin rescue | Essential | Essential (especially at high doses) |
| Myelosuppression | Frequent without rescue | Dose-dependent |
Frequently Asked Questions:
Q1. Is trimetrexate more toxic than methotrexate?
Trimetrexate can be more cytotoxic due to its passive cellular uptake, making leucovorin rescue critically important.
Q2. Can trimetrexate toxicity be reversed?
Yes, with prompt cessation and leucovorin rescue, most toxicities are reversible. However, severe organ damage may have lasting effects.
Q3. How quickly does leucovorin work?
Leucovorin acts rapidly to restore folate pools, with clinical improvement often seen within 24–48 hours.
Q4. Is routine monitoring required during therapy?
Absolutely. CBC, liver function tests, and renal panels should be checked at baseline and throughout treatment.
Q5. Who is most at risk for trimetrexate toxicity?
Patients with pre-existing organ dysfunction, HIV/AIDS, or inadequate leucovorin rescue are at greatest risk.