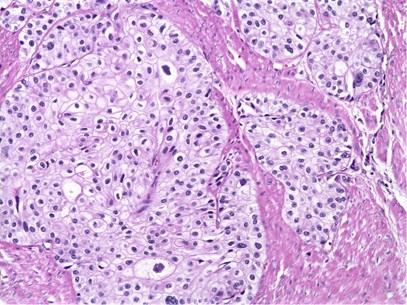
Transitional cell carcinoma (TCC), also known as urothelial carcinoma, is the most prevalent type of cancer affecting the urinary tract. Originating in the urothelium—the specialized epithelial lining of the bladder, ureters, and renal pelvis—TCC accounts for over 90% of bladder cancers and a significant proportion of upper urinary tract malignancies.
This malignancy demonstrates variable behavior, ranging from superficial, non-invasive disease to deeply infiltrative, muscle-invasive tumors with a propensity for metastasis. Early detection and tailored treatment are critical to improving prognosis and quality of life.
Urothelial Anatomy and Origin of TCC
The urothelium is a transitional epithelium capable of stretching and accommodating fluctuating urine volumes. It lines the:
- Renal pelvis
- Ureters
- Urinary bladder
- Proximal urethra
TCC originates from this lining and is capable of arising at any point along the urinary tract, though it most commonly presents in the urinary bladder.
Risk Factors for Transitional Cell Carcinoma
Several modifiable and non-modifiable risk factors contribute to the development of transitional cell carcinoma.
Key Risk Factors
- Tobacco smoking: The leading preventable risk factor due to carcinogenic exposure.
- Occupational exposure: Dyes, rubber, petroleum products, and aromatic amines.
- Chronic urinary tract infections and inflammation
- Long-term use of urinary catheters
- Radiation therapy to the pelvis
- Certain chemotherapy agents (e.g., cyclophosphamide)
- Aristolochic acid exposure (notably linked to upper tract TCC)
- Genetic syndromes such as Lynch syndrome
Clinical Presentation of TCC in the Urinary Tract
Symptoms of Bladder TCC
- Painless hematuria (blood in urine) – the most common presenting symptom
- Frequent urination
- Urgency or dysuria (painful urination)
- Pelvic pain in advanced stages
Symptoms of Upper Tract TCC
- Hematuria
- Flank pain
- Obstructive uropathy leading to hydronephrosis
- Recurrent urinary tract infections
Persistent urinary symptoms or hematuria must prompt thorough urologic evaluation.
Diagnostic Approach to Transitional Cell Carcinoma
Initial Evaluation
- History and physical examination
- Urinalysis and urine cytology
- Imaging:
- Ultrasound (initial bladder assessment)
- CT urography (preferred for upper tract evaluation)
- MRI (alternative in patients with contraindications to CT)
Confirmatory Diagnostics
- Cystoscopy: Direct visualization and biopsy of bladder tumors
- Ureteroscopy: Visualization of ureters and renal pelvis for biopsy
- TURBT (Transurethral Resection of Bladder Tumor): Diagnostic and therapeutic tool for superficial tumors
Histological Grading and Staging of TCC
Accurate classification is essential for prognosis and treatment planning.
Tumor Grading (WHO/ISUP)
- Low-grade: Mild atypia; lower progression risk
- High-grade: Marked atypia; higher recurrence and invasion potential
TNM Staging System
| Stage | Description |
|---|---|
| Ta | Non-invasive papillary carcinoma |
| T1 | Invades subepithelial connective tissue |
| T2 | Invades muscularis propria |
| T3 | Invades perivesical tissue |
| T4 | Invades adjacent organs (e.g., prostate, uterus, pelvic wall) |
Treatment of Transitional Cell Carcinoma
Treatment is guided by the tumor location, grade, and stage. A multidisciplinary approach is often required.
Management of Non-Muscle Invasive Bladder Cancer (NMIBC)
- TURBT followed by:
- Intravesical chemotherapy (e.g., mitomycin C)
- Intravesical immunotherapy (e.g., BCG vaccine)
- Surveillance cystoscopy to monitor recurrence
Management of Muscle-Invasive Bladder Cancer (MIBC)
- Radical cystectomy with urinary diversion
- Neoadjuvant chemotherapy (cisplatin-based)
- Bladder-sparing protocols: Chemoradiation in selected cases
Management of Upper Tract TCC
- Nephroureterectomy: Standard for high-grade or invasive tumors
- Segmental ureterectomy or endoscopic ablation in selected low-grade cases
- Systemic chemotherapy for metastatic disease
Prognosis and Survival Outcomes
Prognostic Factors
- Tumor stage and grade
- Multifocality
- Presence of carcinoma in situ (CIS)
- Lymphovascular invasion
- Patient age and comorbidities
Survival Rates
- 5-year survival for NMIBC: >85%
- 5-year survival for MIBC: ~50%
- Upper tract TCC: Worse prognosis due to later detection; survival depends on early intervention
Recurrence and Surveillance Strategies
Transitional cell carcinoma has a high recurrence rate, especially within the bladder.
Follow-Up Protocols
- Cystoscopy every 3–6 months for NMIBC
- Urine cytology and imaging as indicated
- Annual CT urography for upper tract surveillance post-treatment
Emerging Therapies and Research Trends
- Checkpoint inhibitors (e.g., atezolizumab, nivolumab) for advanced urothelial carcinoma
- Targeted therapies against FGFR mutations
- Gene expression profiling for personalized treatment
- Photodynamic therapy and immune checkpoint blockade in trials
These advances offer hope for improved outcomes, especially in recurrent or refractory cases.
Frequently Asked Questions:
What is transitional cell carcinoma?
Transitional cell carcinoma is a cancer originating from the urothelium, the lining of the bladder, ureters, and renal pelvis.
Is TCC the same as urothelial carcinoma?
Yes, transitional cell carcinoma is now more commonly referred to as urothelial carcinoma.
Can transitional cell carcinoma be cured?
Yes, especially in early-stage disease. Outcomes depend heavily on timely diagnosis and appropriate therapy.
How is TCC detected?
Via urine cytology, cystoscopy, imaging studies, and biopsy.
What is the recurrence risk for TCC?
High, especially in non-muscle invasive bladder cancer. Lifelong surveillance is often necessary.
Transitional cell carcinoma of the urinary tract is a significant urological malignancy requiring early detection and individualized treatment strategies. A comprehensive diagnostic workup, accurate staging, and adherence to evidence-based management protocols are essential to optimizing outcomes. As research continues to unveil targeted therapies and immunotherapeutic options, we anticipate even better prognoses for patients affected by this complex malignancy.