Transfusion reaction urticaria, commonly classified as a mild allergic transfusion reaction, manifests as an acute hypersensitivity response during or shortly after the administration of blood products. It is predominantly characterized by pruritic wheals (hives) and erythema, often without systemic complications. Although generally benign, prompt identification and management are essential to ensure patient safety and to differentiate it from more severe immunologic reactions.
Pathophysiology and Immune Response
The underlying mechanism of transfusion-related urticaria is predominantly IgE-mediated hypersensitivity. Plasma proteins or donor allergens, such as immunoglobulins, haptens, or even trace allergens like peanuts or medications, may trigger mast cell and basophil degranulation in sensitized recipients. This process leads to the release of histamine and other inflammatory mediators, causing vasodilation, increased vascular permeability, and subsequent wheal formation.
Clinical Features of Urticarial Transfusion Reaction
Common Signs and Symptoms
- Sudden onset of pruritus (itching)
- Appearance of raised, erythematous wheals or hives
- Flushing of the skin
- Occasionally mild angioedema
- Occurrence during transfusion or within 1–2 hours post-infusion
Absence of Systemic Involvement
Unlike anaphylactic reactions, urticarial transfusion reactions typically lack respiratory distress, hypotension, fever, or gastrointestinal symptoms, distinguishing them as Grade 1 allergic transfusion reactions under standard classification systems.
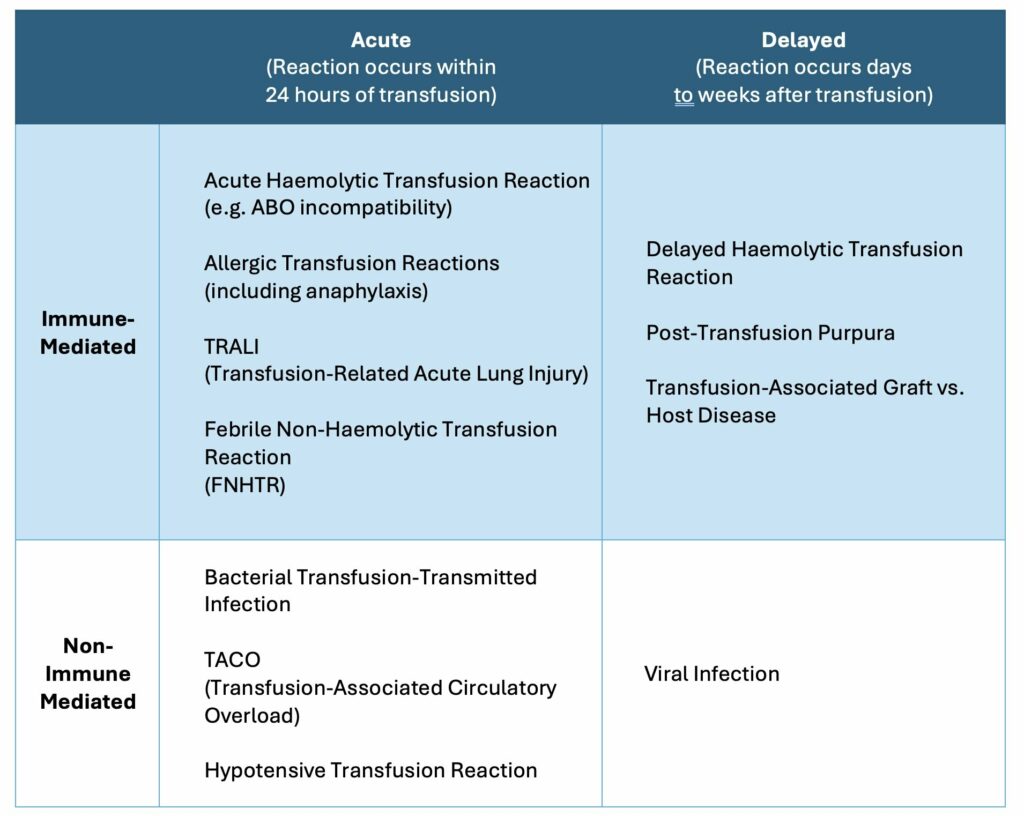
Differential Diagnosis: Distinguishing from Severe Reactions
Proper evaluation is critical to differentiate urticarial transfusion reactions from more serious transfusion complications:
| Condition | Key Features | Systemic Involvement |
|---|---|---|
| Urticarial Reaction | Hives, itching | No |
| Anaphylaxis | Urticaria + hypotension, bronchospasm | Yes |
| Febrile Non-Hemolytic Reaction | Fever, chills | Sometimes |
| Hemolytic Reaction | Hemoglobinuria, back pain, fever | Yes |
An accurate assessment ensures safe continuation of transfusion or rapid escalation of care when necessary.
Risk Factors and Predisposing Conditions
- History of atopy or allergies
- Prior transfusion reactions
- IgA deficiency (especially in anaphylactic risk)
- Repeated transfusions (e.g., thalassemia, sickle cell disease)
- Use of plasma-rich blood products
Sensitized patients may react to minor plasma components even when leukocyte-reduced or washed blood is used.
Management of Transfusion Reaction Urticaria
Immediate Steps
- Stop the transfusion temporarily
- Assess vital signs to rule out systemic involvement
- Administer antihistamines (e.g., diphenhydramine 25–50 mg IV or orally)
- Monitor the patient for symptom resolution
If no additional signs of a severe reaction are present, and symptoms subside, the transfusion may resume with close observation.
Rechallenge and Reinfusion Protocol
- Resume transfusion at a slower rate
- Consider premedication with antihistamines in patients with recurrent reactions
- Ensure availability of emergency medications (e.g., epinephrine) in case of progression
Prevention and Prophylactic Strategies
Premedication
Patients with a history of allergic transfusion reactions may benefit from:
- Antihistamines 30 minutes before transfusion
- In some cases, corticosteroids (e.g., hydrocortisone IV)
Blood Product Modification
- Use of washed red blood cells or platelets to remove residual plasma proteins
- Selection of leukoreduced or plasma-depleted units
These approaches are especially important for patients with multiple prior urticarial reactions or IgA deficiency.
Reporting and Hemovigilance
All transfusion reactions, including mild urticarial responses, should be reported to transfusion services or the hospital’s hemovigilance program. This promotes better data collection, enhances patient safety protocols, and helps guide future transfusion practices.
Key documentation includes:
- Time of onset
- Blood product type
- Lot numbers and donor details
- Symptoms and vital signs
- Intervention and outcome
Prognosis and Outcomes
Urticarial transfusion reactions have an excellent prognosis. Symptoms typically resolve within minutes to a few hours following antihistamine therapy. These reactions do not result in long-term sequelae, but recurrence is possible without preventive strategies.
Repeated urticarial events, however, may necessitate immunohematology consultation and allergen profiling to tailor transfusion strategies effectively.
Frequently Asked Questions
What causes urticaria during blood transfusion?
Urticaria occurs due to an allergic reaction to plasma proteins or allergens in the donor blood, triggering histamine release.
How quickly do symptoms appear?
Symptoms usually begin during transfusion or within 1–2 hours after starting the blood product.
Can transfusion continue after a urticarial reaction?
Yes, if symptoms are mild and resolve with antihistamines, transfusion may continue under close monitoring.
Is this reaction dangerous?
Urticarial transfusion reactions are typically mild. However, any escalation of symptoms must be evaluated to rule out severe complications.
Can it be prevented?
Premedication and the use of washed or plasma-depleted blood components can significantly reduce the risk in susceptible individuals.
Transfusion reaction urticaria, though typically benign, demands a systematic approach to diagnosis, immediate management, and future prevention. Accurate recognition and appropriate response allow safe continuation of transfusion therapy while safeguarding patient well-being. Adoption of prophylactic measures and vigilance in reporting are essential pillars in minimizing recurrence and optimizing transfusion safety.