Trachoma is a highly contagious, chronic eye infection caused by the bacterium Chlamydia trachomatis. It is the leading infectious cause of blindness worldwide. This condition, classified as a neglected tropical disease (NTD), primarily affects populations living in impoverished, overcrowded areas with limited access to clean water and sanitation. The disease is both preventable and treatable, but without timely intervention, it leads to irreversible visual impairment.
Etiology and Transmission of Trachoma
Trachoma is transmitted through:
- Direct contact with ocular or nasal secretions of infected individuals, especially children
- Indirect contact via contaminated clothing, towels, and bedding
- Vectors such as eye-seeking flies (Musca sorbens), which breed in human feces and carry the infection from person to person
Children are the main reservoir of infection, while women, as primary caregivers, face higher risk of repeated exposure, increasing their susceptibility to blinding complications over time.
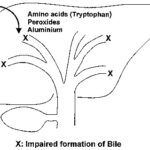
Stages of Trachoma: WHO Grading System
The World Health Organization (WHO) classifies trachoma progression into five distinct stages, collectively known as the WHO simplified grading system:
| Grade | Name | Description |
|---|---|---|
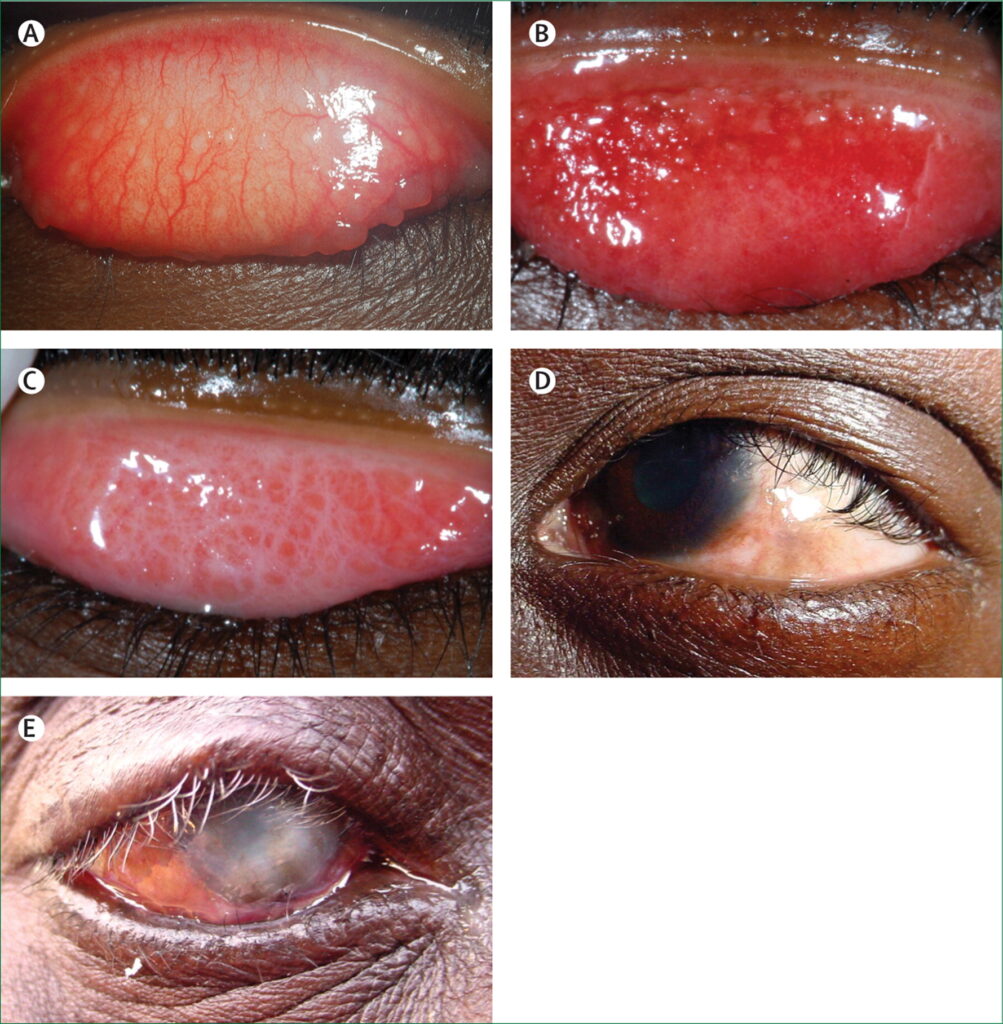
| TF | Trachomatous Inflammation—Follicular | Presence of ≥5 follicles (≥0.5mm) on the upper tarsal conjunctiva |
| TI | Trachomatous Inflammation—Intense | Pronounced thickening and inflammation of the upper conjunctiva |
| TS | Trachomatous Scarring | Scarring of the conjunctival lining of the upper eyelid |
| TT | Trachomatous Trichiasis | Inward turning of eyelashes that scratch the cornea |
| CO | Corneal Opacity | Permanent visual loss due to scarring of the cornea |
Repeated infections throughout childhood lead to scarring and ultimately trachomatous trichiasis, a painful condition where eyelashes turn inward and damage the cornea, potentially resulting in blindness.
Clinical Features and Diagnosis
Early Symptoms
- Redness and irritation in the eyes
- Watery discharge
- Swollen eyelids
- Light sensitivity (photophobia)
- Eye pain
Advanced Disease
- Scarring of the inner eyelid
- Eyelash misdirection (trichiasis)
- Corneal clouding and opacification
- Gradual loss of vision
Diagnostic Approach
Diagnosis is based on clinical examination of the conjunctiva using a magnifying loupe under adequate light, in accordance with WHO grading criteria. In research or complex cases, nucleic acid amplification tests (NAATs) or PCR may be used to confirm Chlamydia trachomatis DNA.
Epidemiology and At-Risk Populations
- Endemic Regions: Sub-Saharan Africa, parts of the Middle East, South Asia, and some regions of Latin America and Oceania
- Global Burden: Over 125 million people live in areas at risk of trachoma, and more than 1.9 million are visually impaired due to the disease
- Vulnerable Groups: Children under 10, women, and individuals in communities lacking adequate sanitation and clean water access
SAFE Strategy: Global Framework for Trachoma Control
The WHO has adopted the SAFE strategy to eliminate trachoma as a public health problem:
| Component | Description |
|---|---|
| S — Surgery | Corrective surgery for trichiasis to prevent blindness |
| A — Antibiotics | Mass administration of azithromycin to eliminate infection |
| F — Facial cleanliness | Promoting hygiene to reduce transmission |
| E — Environmental improvement | Access to clean water, latrines, and proper waste disposal |
The SAFE strategy has shown remarkable success in reducing the prevalence of active trachoma in multiple countries, contributing to elimination in several regions including Morocco, Ghana, and Iran.
Treatment and Management of Trachoma
Pharmacological Treatment
- Azithromycin (single dose): Preferred due to ease of administration and community-wide applicability
- Tetracycline eye ointment: Alternative in areas where azithromycin is unavailable or contraindicated
Surgical Intervention
- Bilateral eyelid surgery (bilamellar tarsal rotation) for trachomatous trichiasis is crucial to prevent corneal damage
- Surgery must be delivered at the community level to increase accessibility and reduce travel burdens on rural populations
Follow-Up Care
Post-treatment, patients require regular check-ups to monitor recurrence and manage complications such as entropion, infection, and corneal opacities.
Prevention of Trachoma: Hygiene and Environmental Control
Effective prevention hinges on breaking the cycle of transmission:
Personal Hygiene
- Encouraging daily face washing among children
- Educating families on hand hygiene practices
- Discouraging eye-touching and sharing of personal items
Community Interventions
- Constructing latrines to reduce open defecation and fly breeding
- Installing water sources near households to enable daily washing
- Proper waste disposal and fly control measures
Trachoma prevention aligns closely with WASH (Water, Sanitation, and Hygiene) initiatives and Sustainable Development Goals (SDGs) aimed at improving global health equity.
Global Progress Toward Elimination
Achievements to Date
- As of 2023, 17 countries have been validated by WHO for eliminating trachoma as a public health problem
- Over 1 billion doses of azithromycin have been distributed through mass drug administration programs
Remaining Challenges
- Political instability, logistical constraints, and limited infrastructure in endemic regions
- Sustained funding and long-term surveillance to prevent resurgence
International cooperation through programs such as WHO’s Alliance for the Global Elimination of Trachoma by 2030 (GET2020) and NGOs like The Carter Center and Sightsavers has been instrumental in these efforts.
Long-Term Outlook and Vision 2030
With intensified implementation of the SAFE strategy, continued pharmaceutical donations (notably azithromycin from Pfizer), and coordinated community efforts, trachoma elimination is within reach. The goal of achieving zero trachoma-related blindness by 2030 is realistic if political will, funding, and health system strengthening persist.
Frequently Asked Questions
What causes trachoma?
Trachoma is caused by repeated infections with the bacterium Chlamydia trachomatis, transmitted via contact with infected secretions or flies.
Can trachoma lead to blindness?
Yes. Chronic or repeated infections result in scarring and inward-turning eyelashes (trichiasis), which scratch the cornea, potentially leading to irreversible blindness.
Is trachoma treatable?
Yes. Early-stage trachoma is treatable with antibiotics. Advanced stages may require surgery to prevent blindness.
How is trachoma prevented?
By promoting facial cleanliness, improving sanitation, ensuring access to clean water, and administering antibiotics in endemic communities.
What is the SAFE strategy?
SAFE stands for Surgery, Antibiotics, Facial cleanliness, and Environmental improvement, a WHO-endorsed approach to eliminate trachoma.
Trachoma remains a preventable yet persistent global health challenge. With coordinated application of the SAFE strategy, integration of WASH programs, and unwavering commitment from international stakeholders, the burden of trachoma can be decisively reduced and ultimately eradicated. Continued awareness, early detection, and community engagement are essential to safeguard vision and improve quality of life in affected regions.