Toxic Epidermal Necrolysis (TEN) is a rare, life-threatening skin disorder characterized by widespread detachment of the epidermis from the dermis. TEN is primarily a drug-induced condition, but can also result from infections or other medical conditions. This condition often presents with a rapid progression of erythematous skin lesions that evolve into blistering and sloughing of the skin, mimicking severe burns. The vast majority of cases are linked to medications, but the underlying pathophysiology is complex and involves immune-mediated mechanisms.
Causes of Toxic Epidermal Necrolysis
1. Drug-Induced Toxic Epidermal Necrolysis
The primary cause of TEN is the use of certain medications. These drugs are believed to trigger a hypersensitivity reaction, often through the activation of cytotoxic T lymphocytes that attack keratinocytes. Some of the most common medications associated with TEN include:
- Antibiotics: Penicillins, sulfonamides, and cephalosporins
- Anticonvulsants: Phenytoin, carbamazepine, lamotrigine
- Allopurinol: Commonly used in the treatment of gout
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Including ibuprofen and diclofenac
- Antiretrovirals: Such as nevirapine
2. Infections and Other Triggers
While drug-induced TEN is most common, viral infections (such as herpes simplex virus or cytomegalovirus) can also trigger TEN in susceptible individuals. Additionally, in rare instances, TEN may be linked to autoimmune conditions like systemic lupus erythematosus or graft-versus-host disease following organ transplants.
3. Genetic Factors
There is emerging evidence suggesting a genetic predisposition to TEN. Certain human leukocyte antigen (HLA) subtypes, particularly HLA-B*1502, have been associated with an increased risk of developing TEN in response to drugs like carbamazepine, particularly in Asian populations.
Pathophysiology of Toxic Epidermal Necrolysis
The pathogenesis of TEN involves an immune-mediated process where drug-induced or infectious antigens activate T cells, which then release cytokines. These cytokines trigger apoptosis (cell death) of keratinocytes in the epidermis. This widespread cell death results in epidermal detachment, leading to the characteristic blistering and sloughing of the skin seen in TEN.
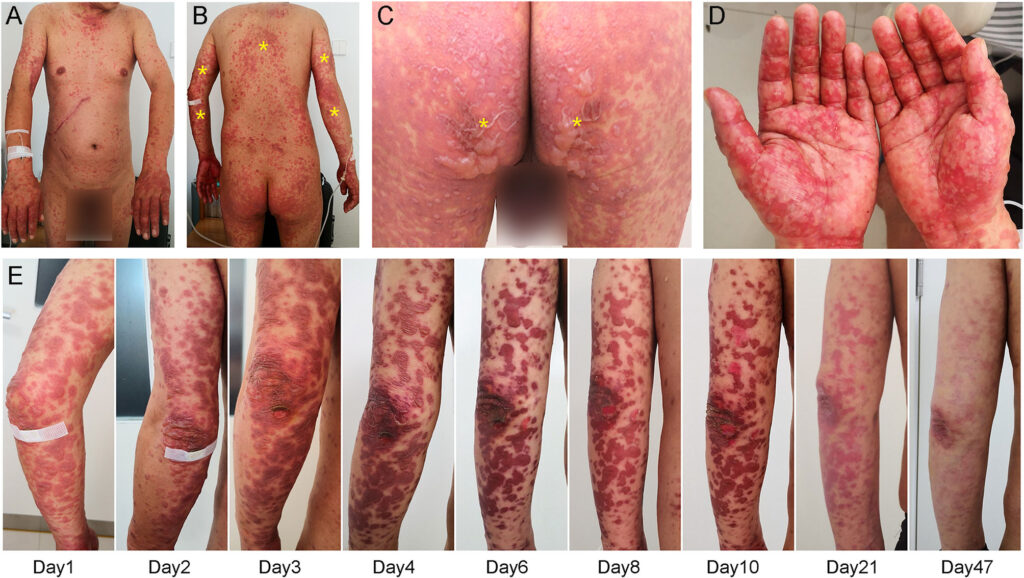
Symptoms of Toxic Epidermal Necrolysis
The clinical presentation of TEN is dramatic and progresses rapidly. Initial symptoms typically begin within a few days to weeks after exposure to a triggering agent.
Early Symptoms:
- Fever: Often the first sign, occurring before skin manifestations
- Malaise and Weakness: Generalized fatigue and discomfort
- Burning Sensation: In the affected areas of the skin, especially on the face and trunk
Skin Manifestations:
- Erythematous Rash: Begins as red, inflamed patches that may become blistered
- Bullous Lesions: Fluid-filled blisters that break easily, leading to erosions
- Epidermal Sloughing: Large sheets of skin begin to peel away, leaving raw, exposed dermis
- Mucosal Involvement: Blistering of mucous membranes, including the eyes, mouth, and genitalia, is common and can lead to severe complications like corneal scarring and gastrointestinal distress
Systemic Symptoms:
- Hypotension: Due to significant fluid loss and skin detachment
- Sepsis: Infection can occur due to the open skin lesions, leading to bacteremia or septic shock
- Organ Dysfunction: Renal, hepatic, or pulmonary complications may arise due to systemic involvement
Diagnosis of Toxic Epidermal Necrolysis
Early diagnosis of TEN is critical for prompt treatment. The diagnosis is primarily clinical, supported by histopathological findings.
Clinical Criteria:
The Nikolsky sign, where the skin easily separates upon gentle pressure, is a key indicator of TEN. If the skin detachment occurs with minimal trauma, this is a strong indicator of TEN.
Histopathology:
Skin biopsy reveals full-thickness epidermal necrosis and subepidermal blistering, which helps confirm the diagnosis. The hallmark of TEN is the separation of the epidermis from the dermis, along with extensive keratinocyte apoptosis.
Laboratory Tests:
- Serum Electrolytes and Renal Function Tests: To assess dehydration and renal involvement
- Blood Cultures: To rule out sepsis
- Liver Function Tests: To evaluate potential liver damage
Differential Diagnosis:
TEN must be distinguished from other severe skin reactions, including:
- Stevens-Johnson Syndrome (SJS): A related condition with similar skin detachment but with less extensive epidermal involvement
- Burns: Trauma or chemical-induced damage to the skin
- Pemphigus Vulgaris: An autoimmune blistering disorder
Treatment of Toxic Epidermal Necrolysis
The management of TEN requires a multidisciplinary approach and prompt intervention to minimize morbidity and mortality.
Immediate Discontinuation of Offending Agents
The first and most crucial step in treating TEN is to immediately discontinue the drug or address the infection that triggered the condition. This can halt the progression of skin detachment and prevent further damage.
Supportive Care:
- Fluid Resuscitation: To replace lost fluids and prevent shock
- Wound Care: Management of skin lesions similar to burn care, including wound cleaning, dressing, and protection from infection
- Pain Management: Pain relief through systemic analgesics and local wound care
- Nutritional Support: Nutritional support is crucial due to significant fluid and electrolyte loss
Immunosuppressive Therapy:
- Corticosteroids: High-dose steroids may be used, although their efficacy remains controversial
- Intravenous Immunoglobulin (IVIG): Some studies suggest that IVIG may help reduce immune-mediated skin damage
- Cyclosporine: Another immunosuppressant used in refractory cases
Monitoring for Complications:
- Sepsis: Vigilant monitoring for signs of infection, including blood cultures and prophylactic antibiotics
- Organ Failure: Regular monitoring of renal, hepatic, and respiratory function
Surgical Interventions:
In severe cases, skin grafting may be necessary once the acute phase has subsided and the patient stabilizes.
Prognosis of Toxic Epidermal Necrolysis
The prognosis of TEN depends on the severity of the condition, the underlying cause, and the timeliness of treatment. Mortality rates have significantly improved with advancements in supportive care and early intervention but can still be as high as 30-40% in severe cases. Complications such as sepsis, multi-organ failure, and long-term mucosal damage may contribute to morbidity.
Factors Affecting Prognosis:
- Age: Elderly patients tend to have worse outcomes
- Extent of Skin Involvement: Greater than 30% body surface area (BSA) involvement is associated with a poorer prognosis
- Delay in Treatment: Delays in recognizing and treating TEN can worsen outcomes
Prevention of Toxic Epidermal Necrolysis
Prevention primarily focuses on avoiding known triggers. Genetic testing may be recommended in certain populations for drugs like carbamazepine to identify individuals at high risk. Additionally, careful monitoring of patients starting new medications, especially those with known risks, can help prevent the development of TEN.
Toxic Epidermal Necrolysis is a severe, life-threatening condition with a high mortality rate, but early diagnosis and prompt, aggressive treatment can significantly improve outcomes. Medical professionals must remain vigilant for the signs of TEN, especially in patients with a history of drug use or infection, and ensure that immediate care focuses on supportive treatment, prevention of infection, and management of complications.