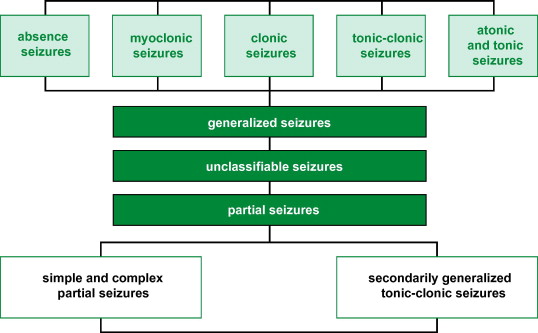
Tonic-clonic epilepsy, a form of generalized epilepsy, often requires adjunctive treatment approaches when first-line monotherapy fails to provide adequate seizure control. Adjunctive therapy refers to **additional interventions—pharmacologic or non-pharmacologic—**that enhance the primary treatment’s effectiveness, reduce seizure frequency, or improve quality of life in patients with drug-resistant or complex seizure profiles.
Indications for Adjunctive Treatment in Generalized Tonic-Clonic Seizures
Adjunctive therapy is typically considered in the following clinical contexts:
- Inadequate seizure control despite optimal dose of a primary antiepileptic drug (AED)
- Drug-resistant epilepsy (DRE) as per ILAE criteria (failure of two appropriate AEDs)
- Presence of intolerable side effects from monotherapy
- Comorbid neurological or psychiatric conditions requiring targeted management
- Improvement of neurocognitive function or mood, which may indirectly influence seizure control
Pharmacological Adjuncts: Second-Line and Add-On Antiepileptic Drugs
When monotherapy is insufficient, combination pharmacotherapy is employed. Careful consideration of drug mechanisms, interactions, and patient-specific factors is essential.
Common Add-On Medications for Tonic-Clonic Seizures
| Adjunct AED | Mechanism of Action | Typical Use Case |
|---|---|---|
| Levetiracetam | SV2A binding, reduces neurotransmitter release | First-line adjunct, minimal interactions |
| Topiramate | GABA enhancement, sodium channel blockade | Effective for generalized seizures |
| Zonisamide | Sodium/calcium channel blocker | Often used in polytherapy |
| Lamotrigine | Sodium channel blocker, glutamate inhibition | Cognitive-friendly adjunct |
| Clobazam | Benzodiazepine derivative, GABA-A modulator | Intermittent use in refractory cases |
| Perampanel | Non-competitive AMPA receptor antagonist | Reserved for resistant generalized seizures |
These agents are introduced incrementally, and plasma drug monitoring may be used in some cases to guide dosing and avoid toxicity.
Non-Pharmacological Adjuncts in Tonic-Clonic Epilepsy Management
In patients with persistent seizures despite adequate pharmacologic treatment, non-drug interventions serve as valuable adjuncts.
Ketogenic and Modified Diet Therapies
- Ketogenic Diet (KD): High-fat, very low-carb, moderate-protein diet shown to significantly reduce seizure frequency.
- Modified Atkins Diet (MAD): Less restrictive alternative, suitable for adolescents and adults.
- Mechanism: Promotes ketosis, altering neuronal excitability via mitochondrial and neurotransmitter pathways.
Neurostimulation Therapies
1. Vagus Nerve Stimulation (VNS)
- Implanted device delivering periodic electrical impulses to the vagus nerve
- Approved for focal and generalized seizures
- Reduces seizure frequency by 30–50% over time
- Beneficial for patients ineligible for surgery
2. Responsive Neurostimulation (RNS)
- Closed-loop device implanted in the skull
- Detects abnormal electrical activity and delivers immediate stimulation
- Currently more effective for focal-onset seizures, but trials continue for generalized forms
3. Deep Brain Stimulation (DBS)
- Targeted stimulation of the anterior nucleus of the thalamus (ANT)
- Emerging option for medically refractory epilepsy with diffuse seizure onset
Biofeedback and Behavioral Approaches
- Neurofeedback training to enhance cortical stability
- Cognitive-behavioral therapy (CBT) to manage stress, anxiety, and improve medication adherence
- Effective as supportive adjuncts in a multidisciplinary epilepsy care model
Surgical Adjuncts: When All Else Fails
In select patients, surgical intervention may serve as the most definitive adjunctive treatment, especially when seizures originate from a resectable focus or become life-threatening.
Corpus Callosotomy
- Indicated in generalized seizures where focal onset cannot be localized
- Surgical disconnection of corpus callosum to prevent seizure spread
- May reduce frequency and severity of drop attacks and generalized seizures
Focal Resection or Lesionectomy
- Less commonly used in tonic-clonic epilepsy unless a focal trigger is identified on EEG/MRI
Hemispherectomy or Hemispherotomy
- Reserved for catastrophic epilepsy syndromes with unilateral structural abnormalities in children
Personalized Medicine and Future Adjunctive Strategies
Pharmacogenomic Profiling
- Identifies individual drug metabolism patterns and potential sensitivities
- Aids in selection of optimal adjunct AEDs
Cannabidiol (CBD)
- Recently approved for certain seizure types, including Lennox-Gastaut and Dravet syndromes
- Investigated as adjunct therapy in broader epilepsy contexts
- Mechanism: Indirect modulation of endocannabinoid system
Investigational Adjuncts
- Gene therapy targeting ion channel disorders
- Stem cell implants for neuroregeneration
- Transcranial magnetic stimulation (TMS) for cortical modulation
Considerations for Effective Adjunctive Therapy
To maximize efficacy, adjunctive treatments must be integrated with:
- Routine follow-ups and drug level monitoring
- Adherence reinforcement
- Comprehensive patient education
- Mental health support
Regular reassessment ensures that adjunctive strategies remain clinically relevant and cost-effective.
Frequently Asked Questions:
What is adjunctive therapy in tonic-clonic epilepsy?
Adjunctive therapy refers to any treatment added to primary AEDs to improve seizure control, including drugs, diets, neurostimulation, or surgery.
When is adjunctive treatment recommended?
It is advised when seizures remain uncontrolled with monotherapy or when side effects necessitate dosage reduction or substitution.
Is the ketogenic diet effective as an adjunct?
Yes, especially in drug-resistant cases. It alters brain metabolism and reduces neuronal hyperexcitability.
What neurostimulation devices are used in epilepsy?
Common devices include VNS, RNS, and DBS, each offering specific benefits based on seizure type and patient profile.
Can surgery be an adjunct treatment?
Yes, particularly when non-resective surgical procedures like corpus callosotomy are used to reduce generalized seizure propagation.
Integrating Adjunctive Therapies in Tonic-Clonic Epilepsy Care
Tonic-clonic epilepsy, especially in drug-resistant forms, requires a multimodal treatment approach. Adjunctive therapies—pharmacological, dietary, surgical, and neurostimulatory—offer valuable options for optimizing seizure control and improving patient outcomes. A personalized, evidence-based regimen combining these adjuncts can significantly elevate the standard of care in epilepsy management.