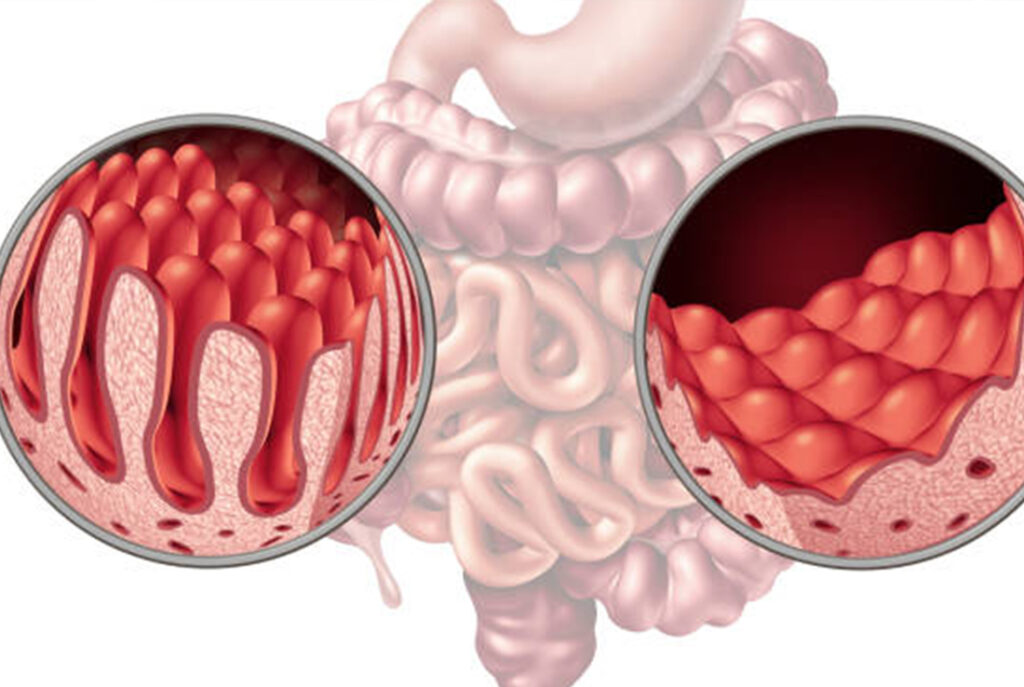
Celiac disease is a chronic autoimmune disorder triggered by the consumption of gluten, a protein found in wheat, barley, and rye. It primarily affects the small intestine, leading to inflammation and damage to the intestinal lining. This damage impairs nutrient absorption, causing a wide range of symptoms and potential complications.
Symptoms
The symptoms of celiac disease vary widely among individuals and can affect multiple organ systems. Common symptoms include:
Digestive Symptoms
- Chronic diarrhea
- Constipation
- Abdominal pain and bloating
- Nausea and vomiting
Non-Digestive Symptoms
- Fatigue
- Weight loss
- Anemia (often due to iron deficiency)
- Bone or joint pain
- Neurological symptoms (e.g., headaches, numbness, or tingling in the hands and feet)
- Skin rash (dermatitis herpetiformis)
Symptoms in Children
- Delayed growth and puberty
- Irritability or behavioral changes
- Dental enamel defects
Causes and Risk Factors
it occurs in genetically predisposed individuals. Specific genes, such as HLA-DQ2 and HLA-DQ8, play a critical role in its development. Environmental factors, such as viral infections or changes in diet, can act as triggers.
Risk Factors Include:
- Having a first-degree relative with celiac disease
- Type 1 diabetes
- Autoimmune thyroid disease
- Down syndrome or Turner syndrome
Diagnosis
Accurate diagnosis is essential to prevent complications. Diagnostic steps include:
1. Medical History and Physical Examination
Doctors assess symptoms, family history, and potential risk factors.
2. Serologic Tests
Blood tests identify specific antibodies, such as:
- tTG-IgA (tissue transglutaminase antibodies)
- EMA (endomysial antibodies)
3. Endoscopy and Biopsy
An endoscopic examination allows doctors to view the small intestine and collect tissue samples to confirm villous atrophy (intestinal damage).
4. Genetic Testing
Testing for HLA-DQ2 and HLA-DQ8 genes helps rule out in uncertain cases.
Important: Do not start a gluten-free diet before completing diagnostic tests, as this can interfere with results.
Managing
The Gluten-Free Diet
The cornerstone of managing celiac disease is adhering to a strict gluten-free diet. Key aspects include:
- Avoiding Gluten-Containing Grains: Eliminate wheat, barley, rye, and derivatives such as malt.
- Choosing Gluten-Free Alternatives: Opt for naturally gluten-free foods like fruits, vegetables, meats, fish, eggs, dairy, rice, and corn.
- Reading Labels: Look for certified gluten-free products and beware of hidden gluten in processed foods, sauces, and medications.
Nutritional Considerations
- Supplement deficiencies in iron, calcium, vitamin D, and B vitamins.
- Increase fiber intake using gluten-free sources like flaxseeds and quinoa.
Monitoring and Follow-Up
Regular follow-ups with healthcare providers ensure proper nutritional status and disease management. Repeat blood tests and symptom assessment help track progress.
Potential Complications
Untreated celiac disease can lead to severe complications, including:
- Malabsorption and associated nutrient deficiencies
- Osteoporosis
- Infertility or pregnancy complications
- Neurological disorders
- Increased risk of intestinal lymphoma and other cancers
Living with Celiac Disease
Tips for Adhering to a Gluten-Free Lifestyle
- Meal Planning: Plan meals to ensure balanced nutrition.
- Dining Out: Communicate dietary needs clearly at restaurants.
- Education: Learn about gluten-containing ingredients and cross-contamination.
Emotional and Social Support
Living with celiac disease can be challenging. Support groups and counseling can provide valuable assistance in adapting to the lifestyle changes required.