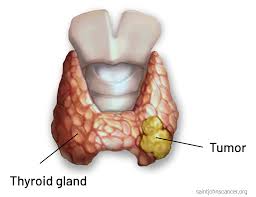
Thyroid carcinoma refers to a malignant tumor arising from the epithelial cells of the thyroid gland. As the most common endocrine malignancy, thyroid cancer has shown a rising incidence globally. While most thyroid carcinomas are indolent and highly treatable, certain aggressive subtypes present significant clinical challenges. Early detection, accurate classification, and a multidisciplinary approach are essential for optimal outcomes.
Types of Thyroid Carcinoma and Their Characteristics
Thyroid carcinomas are categorized based on histological origin and biological behavior. The four primary types include:
1. Papillary Thyroid Carcinoma (PTC)
- Prevalence: ~80% of all thyroid cancers.
- Demographics: Most common in females, aged 30–50.
- Behavior: Slow-growing, often spreads to cervical lymph nodes.
- Histology: Characterized by papillary structures, Orphan Annie eye nuclei, and psammoma bodies.
- Prognosis: Excellent, with >95% 10-year survival rate.
2. Follicular Thyroid Carcinoma (FTC)
- Prevalence: 10–15% of cases.
- Spread: Hematogenous metastasis to bones and lungs, rather than lymph nodes.
- Histology: Uniform follicular cells with capsular and vascular invasion.
- Prognosis: Favorable when diagnosed early; worse with distant metastasis.
3. Medullary Thyroid Carcinoma (MTC)
- Origin: Parafollicular C cells; secretes calcitonin.
- Types: Sporadic (75%) and familial (25%)—linked to RET proto-oncogene mutations.
- Syndromes: May be part of MEN2A or MEN2B.
- Prognosis: Moderate; depends on extent and genetic background.
4. Anaplastic Thyroid Carcinoma (ATC)
- Prevalence: <2%, but accounts for majority of thyroid cancer deaths.
- Presentation: Rapid growth, local invasion, hoarseness, dysphagia.
- Prognosis: Poor; median survival is 6 months.
Pathogenesis and Risk Factors
The development of thyroid carcinoma involves a complex interplay of genetic, environmental, and hormonal factors.
Major Risk Factors
- Radiation exposure during childhood or adolescence.
- Family history of thyroid cancer or genetic syndromes.
- Iodine deficiency (especially associated with follicular carcinoma).
- Benign thyroid diseases such as multinodular goiter or Hashimoto’s thyroiditis.
- Gender and age – higher incidence in women; more aggressive in elderly men.
Clinical Presentation and Symptoms
While many patients are asymptomatic and diagnosed incidentally, common signs include:
- Palpable thyroid nodule
- Neck fullness or pain
- Hoarseness or voice change
- Difficulty swallowing (dysphagia)
- Cervical lymphadenopathy
Red flag symptoms such as rapid nodule growth, vocal cord paralysis, or fixed neck mass suggest aggressive disease and require urgent evaluation.
Diagnostic Approach to Thyroid Carcinoma
1. Thyroid Ultrasound
- First-line imaging for thyroid nodules.
- Evaluates size, composition (solid vs cystic), margins, calcifications, and vascularity.
- High-risk features warrant biopsy.
2. Fine Needle Aspiration Cytology (FNAC)
- Gold standard for nodule evaluation.
- Bethesda classification system guides management:
- Category V-VI: Suspicious/malignant → surgery indicated.
3. Serum Markers
- Thyroglobulin (Tg): Tumor marker for PTC and FTC (post-thyroidectomy surveillance).
- Calcitonin: Marker for medullary thyroid carcinoma.
- CEA: May also be elevated in MTC.
4. Molecular Testing
- Detects mutations in BRAF, RAS, RET/PTC, TERT promoter.
- Assists in risk stratification and surgical planning.
5. Imaging Studies
- CT/MRI: For large tumors or retrosternal extension.
- Radioiodine scan: To detect functional metastases.
- PET-CT: Useful in RAI-refractory or metastatic disease.
Staging of Thyroid Carcinoma
Thyroid cancer is staged using the TNM system (AJCC 8th edition), with age-specific staging applied for differentiated carcinomas (age <55 vs ≥55).
- T (Tumor): Size and invasion extent.
- N (Node): Regional lymph node involvement.
- M (Metastasis): Presence of distant metastasis.
Surgical Management
Surgery is the primary modality for most thyroid carcinomas.
1. Total Thyroidectomy
- Indicated for tumors >1 cm, bilateral disease, nodal metastasis, or aggressive histology.
- Facilitates postoperative RAI therapy and thyroglobulin monitoring.
2. Lobectomy
- Suitable for low-risk, unifocal papillary microcarcinoma (<1 cm).
- May be curative with minimal complications.
3. Central and Lateral Neck Dissection
- Performed in cases with proven nodal metastasis.
Adjuvant Therapy
1. Radioactive Iodine (RAI) Ablation
- Used after thyroidectomy in differentiated thyroid carcinoma (PTC/FTC).
- Destroys residual thyroid tissue and microscopic metastases.
- Not indicated for MTC or ATC.
2. Thyroid Hormone Suppression Therapy
- Suppressive doses of levothyroxine used to lower TSH and prevent recurrence.
- Monitored via TSH and free T4 levels.
3. External Beam Radiation Therapy (EBRT)
- Reserved for unresectable tumors or local recurrence.
- Limited use due to surrounding sensitive structures.
4. Targeted Therapy and Chemotherapy
- Medullary and anaplastic carcinomas may require targeted agents:
- Vandetanib, cabozantinib (MTC)
- Lenvatinib, sorafenib for RAI-refractory cases.
- Cytotoxic chemotherapy has limited efficacy, primarily palliative in ATC.
Prognosis and Survival Rates
Prognosis is excellent for most thyroid carcinomas, especially differentiated types:
| Type | 10-Year Survival Rate |
|---|---|
| Papillary Thyroid Carcinoma | >95% |
| Follicular Thyroid Carcinoma | ~90% |
| Medullary Thyroid Carcinoma | 75–85% (localized) |
| Anaplastic Thyroid Carcinoma | <10% |
Prognostic factors include age, tumor size, extrathyroidal extension, lymph node involvement, and molecular mutations.
Follow-Up and Recurrence Monitoring
- Thyroglobulin levels and neck ultrasound at regular intervals.
- TSH suppression maintained based on recurrence risk.
- RAI scan or PET-CT for suspected recurrence or metastasis.
- Lifelong follow-up is essential due to potential late recurrences.
Frequently Asked Questions:
What is the most common type of thyroid carcinoma?
Papillary thyroid carcinoma is the most common type, accounting for about 80% of all thyroid cancers.
How is thyroid carcinoma diagnosed?
Diagnosis involves ultrasound, fine needle aspiration, serum markers, and sometimes molecular testing and advanced imaging.
Is thyroid cancer curable?
Yes, particularly for papillary and follicular types, which have high survival rates when detected early and treated appropriately.
What are the warning signs of thyroid cancer?
A painless neck mass, voice changes, difficulty swallowing, or rapid growth of a thyroid nodule should prompt immediate evaluation.
Can thyroid carcinoma spread to other organs?
Yes. Papillary and follicular carcinomas may spread to lungs and bones, while anaplastic carcinoma can invade local structures rapidly.
Thyroid carcinoma encompasses a spectrum of malignancies ranging from indolent to highly aggressive. Timely diagnosis, precise histological classification, and a personalized treatment strategy are pivotal to ensuring optimal outcomes. With advances in molecular diagnostics, surgical techniques, and targeted therapies, we can now manage even the most challenging cases with increasing precision and efficacy.