Thrombotic thrombocytopenic purpura (TTP) is a rare, life-threatening hematologic condition characterized by widespread formation of small blood clots (thrombi) in arterioles and capillaries throughout the body. This leads to thrombocytopenia, microangiopathic hemolytic anemia, and multiorgan dysfunction, particularly affecting the brain, kidneys, and heart. Prompt diagnosis and treatment are essential to prevent irreversible organ damage and reduce mortality.
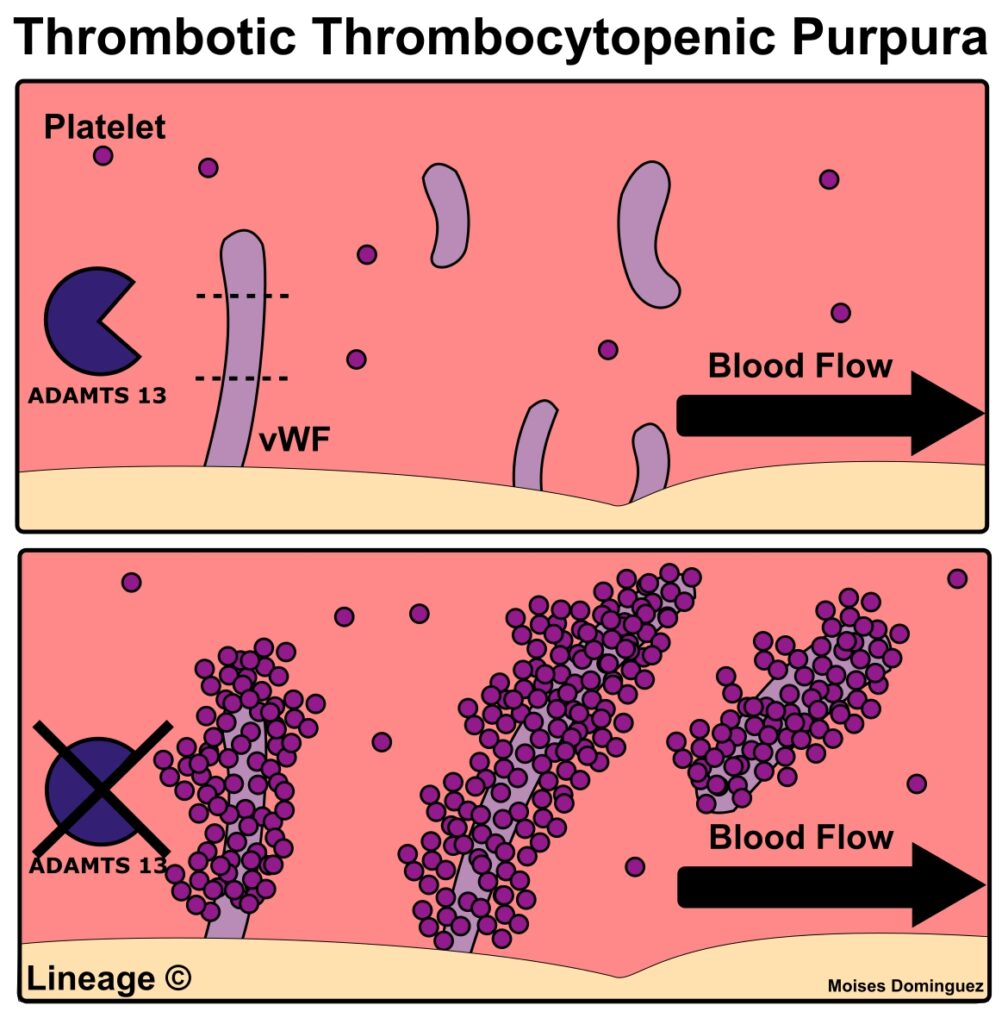
Pathogenesis: The Role of ADAMTS13 in TTP
At the molecular level, TTP results from a severe deficiency of ADAMTS13, a metalloprotease enzyme responsible for cleaving ultra-large von Willebrand factor (vWF) multimers. When ADAMTS13 activity is deficient—either due to an autoimmune inhibitor (acquired TTP) or genetic mutations (congenital TTP)—these ultra-large vWF multimers accumulate, leading to spontaneous platelet aggregation and widespread microvascular thrombosis.
Classification of TTP
Acquired TTP
- Autoimmune form caused by autoantibodies that inhibit ADAMTS13.
- Most common form in adults.
- Often associated with conditions like lupus, infections, pregnancy, and certain medications (e.g., quinine, ticlopidine).
Congenital TTP (Upshaw–Schulman Syndrome)
- Inherited autosomal recessive condition caused by mutations in the ADAMTS13 gene.
- Manifests in infancy or early childhood.
- May present episodically and is often triggered by infection or stress.
Clinical Features and Symptoms of TTP
The classic pentad of TTP includes:
- Thrombocytopenia – causing bruising, petechiae, or bleeding.
- Microangiopathic hemolytic anemia – marked by fatigue, pallor, jaundice.
- Neurological symptoms – confusion, headache, stroke, seizures, coma.
- Renal dysfunction – elevated creatinine, hematuria, proteinuria.
- Fever – non-specific and may be absent in many cases.
In current clinical practice, most patients present with only the first two features, which are sufficient to suspect TTP.
Diagnostic Evaluation of TTP
Laboratory Tests
- Peripheral blood smear: Schistocytes (fragmented RBCs) indicative of microangiopathy.
- Complete blood count (CBC): Low platelet count and hemoglobin.
- Lactate dehydrogenase (LDH): Elevated due to hemolysis.
- Indirect bilirubin: Elevated.
- Reticulocyte count: Elevated due to bone marrow compensation.
- Coombs test: Negative (helps differentiate from autoimmune hemolytic anemia).
- Creatinine and BUN: Assess renal involvement.
Specific Testing for ADAMTS13
- ADAMTS13 activity level: <10% is diagnostic of TTP.
- ADAMTS13 inhibitor test: Confirms acquired TTP if autoantibodies are present.
Differential Diagnosis of TTP
Given its overlapping features with other thrombotic microangiopathies, TTP must be distinguished from:
- Hemolytic uremic syndrome (HUS)
- Disseminated intravascular coagulation (DIC)
- Systemic lupus erythematosus (SLE)
- Malignant hypertension
- Heparin-induced thrombocytopenia (HIT)
Emergency Management and First-Line Treatment
Plasma Exchange Therapy (PEX)
The cornerstone of treatment for acquired TTP is daily plasma exchange (PEX):
- Removes circulating anti-ADAMTS13 autoantibodies.
- Replaces deficient ADAMTS13 with donor plasma.
- Initiated immediately upon suspicion, even before confirmation.
Corticosteroids
- Prednisone or methylprednisolone is used concurrently with PEX to suppress immune-mediated ADAMTS13 inhibition.
Adjunctive and Targeted Therapies
Rituximab
- Anti-CD20 monoclonal antibody used for refractory or relapsing acquired TTP.
- Depletes B cells that produce ADAMTS13 autoantibodies.
- Can be administered during acute episodes or as prophylaxis against recurrence.
Caplacizumab
- Anti-vWF nanobody approved for acquired TTP.
- Inhibits interaction between vWF and platelets, reducing microthrombus formation.
- Used in conjunction with PEX and immunosuppression.
FFP Infusions in Congenital TTP
- In Upshaw–Schulman syndrome, plasma infusions replenish ADAMTS13 and are used prophylactically or during acute episodes.
Monitoring and Long-Term Management
- Platelet counts are monitored daily during the acute phase.
- LDH and hemoglobin levels assess hemolysis resolution.
- ADAMTS13 activity is followed after treatment to detect relapse risk.
Prevention of Recurrence
- Maintenance rituximab or immunosuppressants in high-risk patients.
- Regular ADAMTS13 monitoring every 3–6 months.
Prognosis and Outcomes
Before PEX, the mortality rate of TTP exceeded 90%. With early recognition and treatment, survival now exceeds 85–90%. However, relapses occur in approximately 30–50% of cases and necessitate long-term follow-up.
Frequently Asked Questions:
What triggers thrombotic thrombocytopenic purpura?
Triggers include infections, autoimmune diseases, pregnancy, certain drugs, and stress. Congenital forms may be triggered by febrile illness or trauma.
Is TTP curable?
While there is no absolute cure, most patients achieve complete remission with prompt treatment. Lifelong monitoring is essential for early relapse detection.
Can TTP recur?
Yes. Both acquired and congenital forms can recur. Recurrence is more common in acquired TTP, especially if ADAMTS13 activity remains low after treatment.
How is TTP different from HUS?
TTP primarily affects the central nervous system, while HUS (hemolytic uremic syndrome) more commonly involves the kidneys and is often caused by shiga-toxin-producing bacteria.
Is plasma exchange always necessary?
Yes, in acquired TTP, PEX is life-saving and must be initiated immediately upon clinical suspicion, even before ADAMTS13 results are available.
Thrombotic thrombocytopenic purpura is a medical emergency that demands prompt recognition and intervention. Characterized by ADAMTS13 deficiency and systemic microvascular thrombosis, TTP requires a high index of suspicion and early treatment with plasma exchange, immunosuppressants, and emerging therapies like caplacizumab. Ongoing monitoring and individualized long-term management remain essential to prevent recurrence and ensure patient survival.