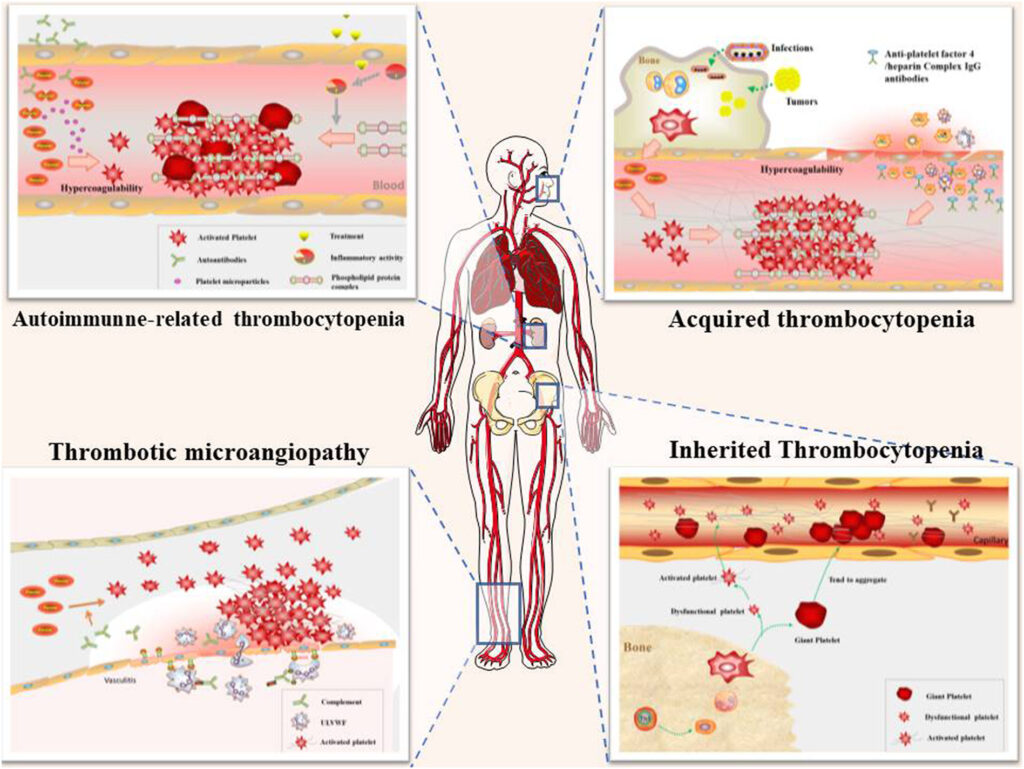
Thrombosis with thrombocytopenia syndrome (TTS) is a rare but life-threatening condition characterized by the combination of blood clots (thrombosis) and a low platelet count (thrombocytopenia). TTS has garnered global attention due to its association with certain adenoviral vector-based COVID-19 vaccines, though it can also occur independently or as part of autoimmune conditions.
TTS shares pathological features with heparin-induced thrombocytopenia (HIT), including platelet activation by antibodies against platelet factor 4 (PF4), even in the absence of heparin exposure. Timely recognition and appropriate management are crucial to prevent fatal outcomes.
Etiology and Risk Factors of TTS
Immune-Mediated Mechanisms
The underlying mechanism in TTS is immune-mediated platelet activation. Autoantibodies target PF4, leading to excessive platelet aggregation and paradoxical thrombus formation despite thrombocytopenia. The process mimics HIT but is triggered by non-heparin antigens, such as vaccine components or other stimuli.
Identified Triggers
- Adenoviral vector vaccines (e.g., ChAdOx1 nCoV-19, Ad26.COV2.S)
- Autoimmune disorders
- Certain medications
- Genetic predispositions
Demographics at Elevated Risk
- Women under 50 years of age
- Individuals with prior autoimmune conditions
- Patients with a history of venous thromboembolism
Clinical Manifestations and Thrombotic Complications
Common Symptoms
- Severe headache or neurologic deficits (suggesting cerebral venous sinus thrombosis)
- Abdominal pain (possible splanchnic vein thrombosis)
- Leg swelling (deep vein thrombosis)
- Chest pain and dyspnea (pulmonary embolism)
- Petechiae or unusual bleeding due to thrombocytopenia
Thrombotic Sites
- Cerebral venous sinus thrombosis (CVST)
- Splanchnic vein thrombosis
- Pulmonary embolism
- Arterial thrombosis (less frequent)
Diagnostic Criteria and Laboratory Investigations
Diagnostic Criteria (per WHO and CDC guidance)
- Acute onset of thrombosis (especially in atypical locations)
- Thrombocytopenia (platelets <150×10⁹/L)
- Onset 4–30 days post-exposure to potential trigger (commonly a vaccine)
- Positive PF4-polyanion ELISA assay
- No prior heparin exposure (or temporal dissociation from heparin use)
Recommended Investigations
- Complete blood count: Assess platelet count
- D-dimer: Elevated significantly
- Fibrinogen: May be reduced
- Immunoassays for PF4 antibodies: ELISA preferred
- Imaging: MRI/MRV for cerebral thrombosis, abdominal CT for splanchnic thrombosis
Differential Diagnosis
- Heparin-induced thrombocytopenia (HIT): History of heparin use required
- Antiphospholipid syndrome
- Thrombotic thrombocytopenic purpura (TTP)
- Disseminated intravascular coagulation (DIC)
Distinguishing TTS requires exclusion of heparin exposure and confirmation of PF4 antibody presence through ELISA, not just functional HIT assays.
Evidence-Based Management of TTS
Initial Stabilization
- Hospital admission with ICU monitoring if cerebral or abdominal thrombosis suspected
- Avoid platelet transfusions unless clinically necessary for life-threatening hemorrhage
Anticoagulation Strategy
Non-heparin anticoagulants are mandatory.
- Direct thrombin inhibitors: Argatroban, bivalirudin
- Factor Xa inhibitors: Fondaparinux, apixaban, rivaroxaban
Initiate anticoagulation as soon as TTS is suspected, even before confirmatory testing, unless contraindicated by active bleeding.
Immunomodulatory Therapy
- Intravenous immunoglobulin (IVIG): 1 g/kg/day for 2 days
- Steroids: High-dose methylprednisolone if IVIG unavailable or insufficient
- Plasmapheresis: Considered in refractory cases
Long-Term Management and Prognosis
Duration of Anticoagulation
- Minimum of 3 months anticoagulation for confirmed thrombosis
- Longer duration in persistent thrombocytopenia or repeated antibody positivity
Monitoring Parameters
- Platelet count until normalization
- D-dimer and fibrinogen for coagulation status
- Serial imaging if clinically indicated
Prognosis
- Mortality rates range from 20% to 50% if untreated
- Early recognition and treatment significantly improve outcomes
- Patients recovering from TTS may receive mRNA-based vaccines for future immunizations
Prevention and Patient Education
Vaccine Risk Communication
- TTS risk remains extremely rare (estimated at <1 per 100,000 vaccine doses)
- Benefits of vaccination outweigh risks in nearly all populations
Patient Counseling
- Prompt reporting of post-vaccine symptoms (persistent headache, abdominal pain, leg swelling)
- Avoiding heparin products in future unless testing confirms lack of PF4-reactive antibodies
Frequently Asked Questions:
Is TTS the same as HIT?
No. TTS is a heparin-independent syndrome with similar pathophysiology to HIT but occurs without prior heparin exposure. Both involve PF4-reactive antibodies.
Which vaccines are associated with TTS?
Adenovirus-based vaccines such as AstraZeneca’s ChAdOx1 nCoV-19 and Johnson & Johnson’s Ad26.COV2.S have been linked to rare TTS cases.
What is the treatment of choice for TTS?
IVIG and non-heparin anticoagulation are the mainstays of treatment. Heparin use must be strictly avoided.
Can patients with past TTS be vaccinated again?
Yes, but mRNA vaccines (e.g., Pfizer-BioNTech, Moderna) are preferred and considered safe post-recovery from TTS.
What is the diagnostic gold standard for TTS?
Positive PF4-polyanion ELISA with clinical symptoms of thrombosis and thrombocytopenia, in the absence of heparin exposure.
Thrombosis with thrombocytopenia syndrome is a rare but medically urgent condition with high morbidity and mortality if unrecognized. Prompt diagnosis, cessation of heparin, initiation of appropriate anticoagulation, and immune modulation are essential. Widespread awareness, rapid action, and evidence-based protocols remain key to ensuring optimal patient outcomes in TTS management.