Heparin-induced thrombocytopenia (HIT) is a severe prothrombotic immune complication of heparin exposure, particularly concerning in the setting of percutaneous coronary intervention (PCI). Despite its thrombocytopenic nature, HIT leads to paradoxical thrombosis that can compromise coronary perfusion, cause stent thrombosis, and lead to catastrophic outcomes during interventional procedures. A meticulous approach is required to safely manage these patients during PCI.
Pathogenesis of HIT and Thrombotic Risk During PCI
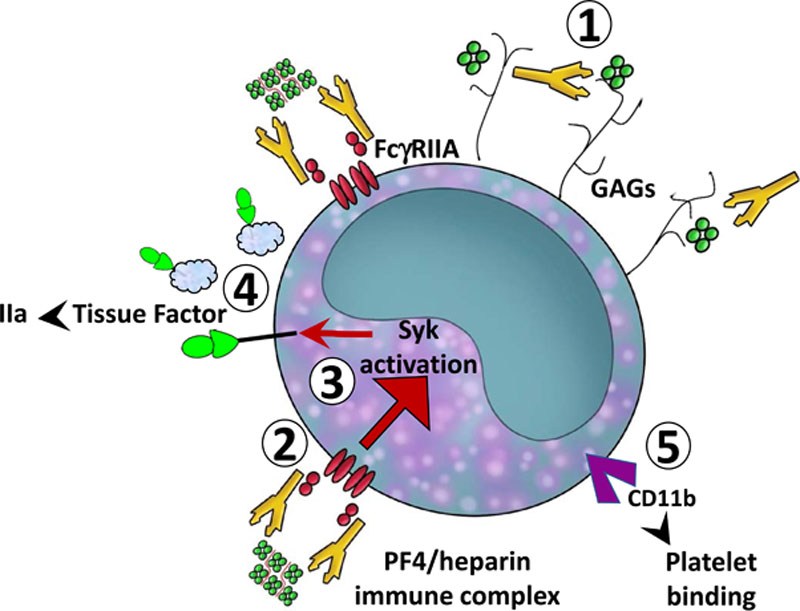
HIT occurs when heparin binds to platelet factor 4 (PF4), forming an immunogenic complex that stimulates IgG antibody production. These antibodies activate platelets, leading to widespread thrombin generation. During PCI, where vascular injury and platelet activation are already elevated, HIT exponentially increases thrombotic risk.
Clinical Presentation and Diagnosis in the PCI Setting
Early Identification
Patients may present with:
- Abrupt platelet count drop (typically >50%)
- New thrombotic complications post-heparin exposure
- Resistance to heparin anticoagulation during PCI
- Acute stent thrombosis or myocardial infarction without mechanical cause
Diagnostic Tools
- 4Ts score: Risk stratification prior to intervention
- PF4/heparin antibody ELISA: High sensitivity
- Functional assays (SRA, HIPA): High specificity, confirmatory
In urgent PCI settings, rapid immunoassays are useful to guide immediate decisions.
Safe PCI Strategies in HIT-Positive or Suspected Patients
Discontinuation of All Heparin Products
Immediate cessation of all heparin forms is crucial, including heparin flushes and low molecular weight heparin (LMWH).
Alternative Anticoagulation Agents During PCI
1. Argatroban
- Direct thrombin inhibitor
- Hepatic clearance
- Short half-life
- Preferred in patients with renal dysfunction
2. Bivalirudin
- Direct thrombin inhibitor
- Rapid onset and short half-life
- Ideal for high-risk coronary interventions
- Lower bleeding risk than argatroban
3. Fondaparinux (off-label)
- Factor Xa inhibitor
- Not typically used during PCI due to risk of catheter thrombosis unless supplemented with procedural anticoagulants
Dosing and Monitoring
- Argatroban: Start at 350 μg/kg bolus, then 25 μg/kg/min infusion; titrate to maintain ACT >300s during PCI
- Bivalirudin: 0.75 mg/kg IV bolus followed by 1.75 mg/kg/h infusion during PCI
Intraoperative Management Considerations
Activated Clotting Time (ACT) Monitoring
- ACT must be closely monitored to ensure adequate anticoagulation.
- Delays or inadequate ACT adjustment increase stent thrombosis risk in HIT patients.
Procedural Adjustments
- Use of radial access to minimize bleeding complications
- Shorter procedural times where possible
- Meticulous catheter handling to avoid mechanical thrombosis
Post-PCI Antithrombotic Management
Transitioning to Long-Term Anticoagulation
- Continue non-heparin anticoagulant post-PCI until platelet count recovery
- Consider direct oral anticoagulants (DOACs) for extended therapy if stable
- Warfarin should not be started until platelet count >150 x 10⁹/L
Dual Antiplatelet Therapy (DAPT)
- Standard DAPT (aspirin + P2Y12 inhibitor) continues as per stent type
- Does not replace anticoagulation in HIT-positive patients
Special Populations and High-Risk Scenarios
Emergent PCI in Suspected HIT
- Use bivalirudin or argatroban immediately
- Send HIT panel but do not delay PCI if STEMI or unstable angina
Patients with HIT and Renal Dysfunction
- Argatroban preferred due to hepatic clearance
- Bivalirudin requires renal dose adjustment
HIT with Active Thrombosis and High Bleeding Risk
- Short-duration bivalirudin followed by oral anticoagulants
- Avoid heparin exposure in any form
Outcomes and Prognosis
Thrombosis due to HIT during PCI carries a high risk of mortality, myocardial infarction, and limb-threatening ischemia. However, with rapid identification and proper anticoagulation strategy, procedural success rates are comparable to standard PCI cases.
Key Prognostic Indicators:
- Time to HIT recognition
- Speed and adequacy of anticoagulation switch
- Early thrombosis management
- Comorbid renal or hepatic dysfunction
Frequently Asked Questions:
What is the best anticoagulant for HIT during PCI?
Bivalirudin is often preferred for its rapid action, short half-life, and favorable bleeding profile. Argatroban is ideal in patients with renal impairment.
Can heparin be used in HIT patients during PCI with pre-treatment?
No. All heparin forms, including low-dose or LMWH, must be avoided due to risk of rapid and fatal thrombosis.
How is anticoagulation monitored during HIT-positive PCI?
Activated Clotting Time (ACT) is used intraoperatively to guide dosing of direct thrombin inhibitors like bivalirudin or argatroban.
What is the role of dual antiplatelet therapy in HIT-related PCI?
DAPT remains necessary post-PCI for stent protection but does not replace systemic anticoagulation in HIT patients.
Can DOACs be used post-PCI in HIT patients?
Yes, DOACs such as apixaban or rivaroxaban are emerging as viable options after platelet count recovery, especially in stable cases.
Managing thrombosis associated with heparin-induced thrombocytopenia during PCI demands rapid diagnosis, elimination of heparin, and expert selection of alternative anticoagulation. With adherence to evidence-based protocols, safe and effective coronary interventions are achievable even in this high-risk patient population.