Heparin-induced thrombocytopenia (HIT) is a life-threatening, immune-mediated complication of heparin therapy, characterized by a significant drop in platelet count and an increased risk of thrombosis. Paradoxically, despite thrombocytopenia, patients with HIT are at an exceptionally high risk of both arterial and venous thrombotic events. Prompt diagnosis and intervention are critical to reducing morbidity and mortality.
Pathophysiology of HIT-Associated Thrombosis
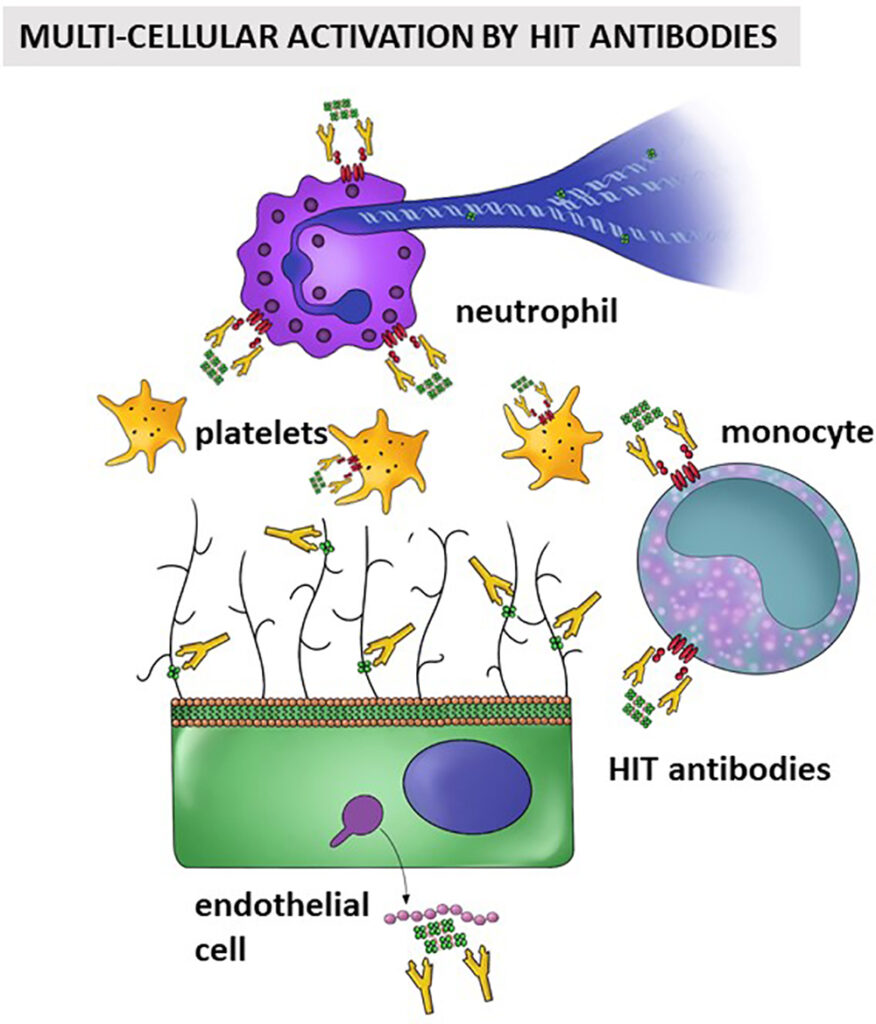
HIT occurs when heparin binds to platelet factor 4 (PF4), forming a complex that triggers an autoimmune response. The resulting anti-PF4/heparin antibodies activate platelets, leading to a prothrombotic state. This cascade results in widespread platelet consumption and a heightened risk of thrombosis.
Diagnosing HIT Before Thrombotic Events Occur
Clinical Suspicion and Scoring
The 4Ts score (Thrombocytopenia, Timing, Thrombosis, oTher causes) is an essential diagnostic tool. A high score necessitates immediate cessation of heparin and further laboratory confirmation.
Laboratory Testing
- ELISA for anti-PF4/heparin antibodies – High sensitivity
- Functional assays such as serotonin release assay (SRA) – High specificity
- Rapid immunoassays for bedside decision-making
Immediate Actions Upon HIT Diagnosis
Discontinuation of All Heparin Products
Heparin cessation is the cornerstone of HIT management. This includes intravenous, subcutaneous, catheter flushes, and heparin-coated devices.
Initiation of Non-Heparin Anticoagulation
Since HIT is prothrombotic, patients require alternative anticoagulation even in the absence of thrombosis. Recommended agents include:
- Argatroban – Direct thrombin inhibitor, hepatic clearance
- Bivalirudin – Short half-life, especially useful perioperatively
- Fondaparinux – Indirect factor Xa inhibitor, off-label but increasingly favored
- DOACs (rivaroxaban, apixaban) – Emerging evidence supports use in stable patients
Strategies for Thrombosis Prevention in HIT
Risk Stratification and Monitoring
- Daily platelet counts in patients on heparin >5 days
- Early identification in high-risk populations (post-surgical, cardiovascular)
- Ultrasound screening for deep vein thrombosis (DVT) in HIT-positive patients
Avoiding Platelet Transfusions
Platelet transfusions are contraindicated unless there is life-threatening bleeding due to the risk of exacerbating thrombosis.
Optimal Dosing and Monitoring of Anticoagulants
- Argatroban: Adjust dose based on aPTT; beware of falsely elevated INR
- Fondaparinux: Once daily subcutaneous, minimal monitoring needed
- DOACs: Appropriate only after platelet count recovery (>150 x 10⁹/L)
Transitioning to Long-Term Anticoagulation
When and How to Initiate Warfarin
- Begin only after platelet recovery to >150 x 10⁹/L
- Overlap with non-heparin anticoagulant for at least 5 days
- INR must be therapeutic (2.0–3.0) for 2 consecutive days before stopping the parenteral agent
DOACs as Alternatives
In select cases, direct oral anticoagulants may serve as both acute and maintenance therapy, particularly when monitoring resources are limited.
Special Considerations
HIT in Surgical and Critical Care Patients
- Prefer short-acting agents like bivalirudin perioperatively
- Monitor for thrombotic events postoperatively despite anticoagulation
HIT with Thrombosis (HITT)
Patients with HITT require at least 3 months of anticoagulation. Therapy choice and duration depend on clot burden and bleeding risk.
Pediatric and Pregnant Patients
- Danaparoid and fondaparinux are safer alternatives in pregnancy
- Data in pediatric populations are limited; specialist consultation advised
Prognosis and Long-Term Management
- Mortality in untreated HIT with thrombosis may exceed 20%
- With prompt intervention, risk decreases significantly
- Long-term anticoagulation reduces recurrence
- Re-exposure to heparin must be documented as contraindicated
Preventing thrombosis in heparin-induced thrombocytopenia requires early recognition, immediate heparin cessation, and initiation of alternative anticoagulation. Precision in diagnosis, appropriate therapeutic selection, and vigilant monitoring are paramount in minimizing thrombotic complications and improving patient outcomes.