CD30-positive mycosis fungoides (MF) represents a rare subtype of cutaneous T-cell lymphoma (CTCL) characterized by the overexpression of the CD30 protein on tumor cells. This condition often presents unique clinical features and requires specialized diagnostic and therapeutic approaches. This article provides an in-depth examination of CD30-positive mycosis fungoides, addressing its pathophysiology, clinical presentation, diagnostic criteria, treatment options, and prognosis.
Pathophysiology and CD30 Expression
CD30, a member of the tumor necrosis factor (TNF) receptor superfamily, is a transmembrane protein commonly associated with Hodgkin lymphoma and certain subtypes of CTCL. In CD30-positive MF, the aberrant expression of this marker is linked to tumor progression and immune evasion.
- CD30 Marker Role: CD30 positivity indicates activated T cells and can distinguish aggressive MF subtypes from indolent variants.
- Molecular Pathways: The activation of CD30-associated signaling pathways, such as NF-κB, promotes cell proliferation and survival.
- Clinical Relevance: The degree of CD30 expression may influence therapeutic decisions and correlate with disease outcomes.
Clinical Presentation
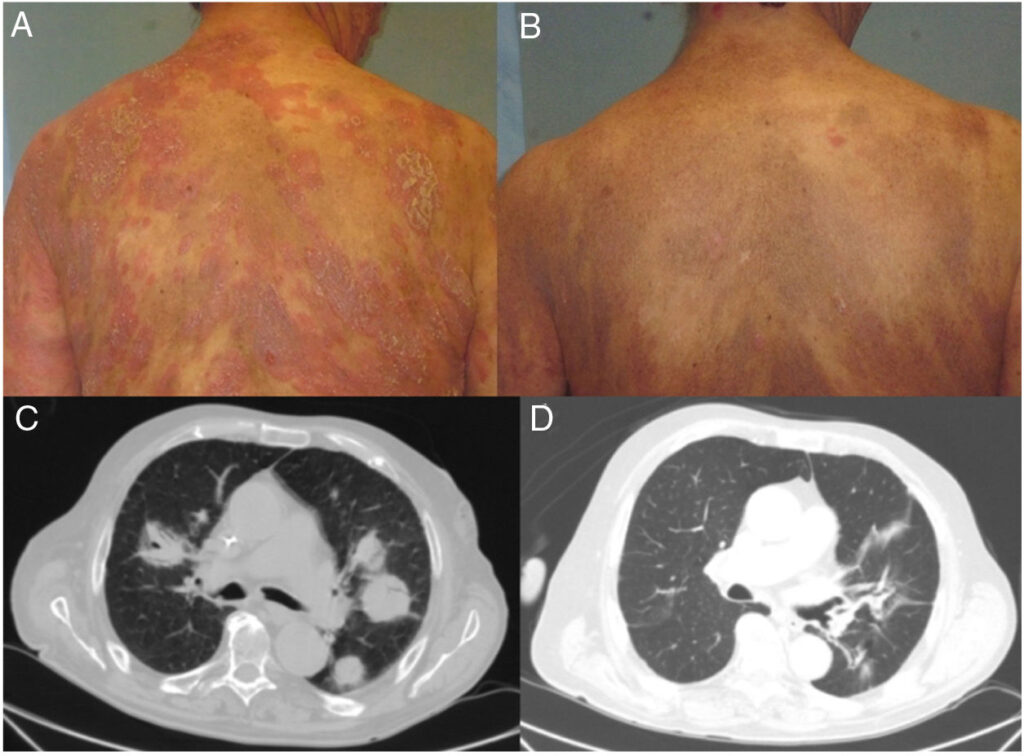
Patients with CD30-positive MF may exhibit a broad spectrum of skin lesions, ranging from patches and plaques to nodules and tumors. Key clinical features include:
- Patch-Stage MF: Scaly, erythematous lesions that may be asymptomatic or mildly pruritic.
- Tumor-Stage MF: Nodular lesions with or without ulceration, often indicative of advanced disease.
- CD30 Variability: The intensity and distribution of CD30-positive cells vary among patients, contributing to heterogeneous clinical behavior.
Diagnostic Approach
Accurate diagnosis of CD30-positive MF necessitates a combination of clinical, histopathological, and immunophenotypic evaluations.
1. Histopathology
- Epidermotropism with atypical lymphocytes.
- Dermal infiltrates rich in CD30-positive tumor cells.
- Absence of significant eosinophils or neutrophils.
2. Immunohistochemistry
- CD30 expression is detected using monoclonal antibodies.
- Positive staining in ≥30% of tumor cells confirms CD30 positivity.
- Co-expression of T-cell markers such as CD3 and CD4.
3. Molecular Studies
- T-Cell Receptor (TCR) Clonality: Identifies monoclonal T-cell populations.
- Gene Expression Profiling: Differentiates aggressive variants.
Treatment Strategies
The management of CD30-positive mycosis fungoides varies based on disease stage and CD30 expression levels. Standard treatments include:
1. Skin-Directed Therapies
- Topical Corticosteroids: Effective for early-stage patches and plaques.
- Phototherapy: Narrowband UVB or PUVA.
- Localized Radiation Therapy: For refractory lesions.
2. Systemic Therapies
- Brentuximab Vedotin: An anti-CD30 antibody-drug conjugate demonstrating efficacy in CD30-positive lymphomas.
- Chemotherapy: Reserved for advanced or refractory cases.
- Immunomodulatory Agents: Interferons or retinoids.
3. Emerging Therapies
- Checkpoint inhibitors targeting PD-1/PD-L1 pathways.
- CAR-T cell therapies specific to CD30.
Prognosis and Outcomes
The prognosis of CD30-positive mycosis fungoides is highly variable and depends on several factors, including:
- Disease Stage: Early-stage MF has a favorable prognosis compared to advanced disease.
- CD30 Expression Levels: Higher levels correlate with aggressive behavior but may also predict better responses to CD30-targeted therapies.
- Treatment Response: Complete remission is achievable in localized disease but less common in advanced stages.
Survival Rates
- Early-Stage Disease: 5-year survival exceeds 90%.
- Advanced Disease: 5-year survival ranges between 40%-60%.