Abdominal Hysterectomy Infection Prevention is a critical component of care for patients undergoing abdominal hysterectomy. Ensuring proper protocols and practices can significantly reduce postoperative complications and enhance recovery outcomes. This article provides a detailed overview of strategies for minimizing infection risk associated with abdominal hysterectomy.
Understanding Abdominal Hysterectomy and Infection Risks
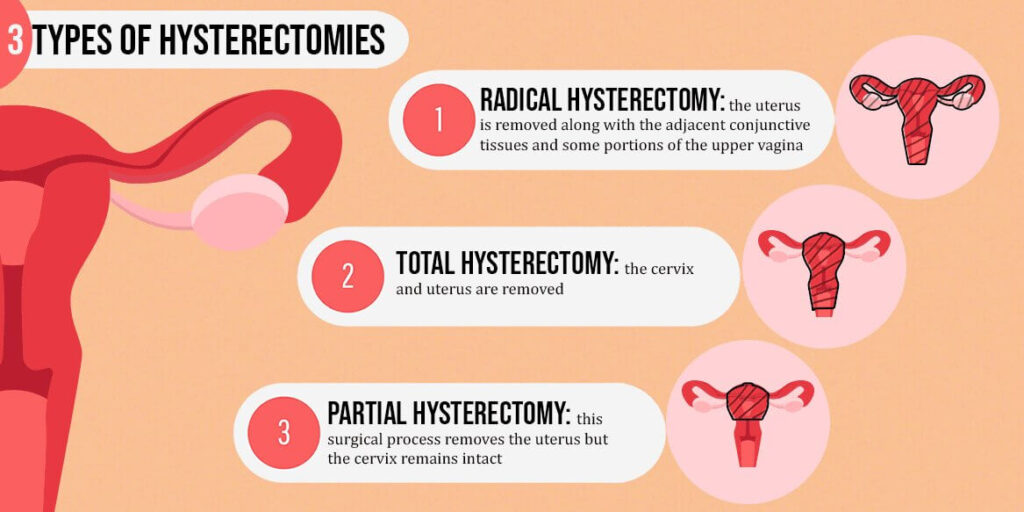
An abdominal hysterectomy involves the surgical removal of the uterus through an incision in the abdomen. Despite advancements in surgical techniques, this procedure carries inherent risks of infection due to the involvement of internal organs and tissues.
Common Infection Types
- Surgical Site Infections (SSIs): Infections at the incision site or deeper within the abdominal cavity.
- Urinary Tract Infections (UTIs): Often related to catheterization during or after surgery.
- Sepsis: A rare but severe systemic infection.
Risk Factors
- Pre-existing medical conditions, such as diabetes or obesity.
- Prolonged surgery duration.
- Poor nutritional status or immune compromise.
- Inadequate preoperative preparation.
Preoperative Infection Prevention Strategies
Comprehensive Patient Assessment
Evaluating the patient’s medical history and overall health is the first step in infection prevention. Key considerations include:
- Identifying comorbidities that may increase infection risks.
- Conducting blood tests to detect anemia or other deficiencies.
- Screening for potential sources of infection, such as dental or urinary tract infections.
Skin Preparation
Proper skin preparation reduces microbial load at the surgical site. Recommended practices include:
- Preoperative Showering: Use of chlorhexidine-based antiseptic solutions.
- Hair Removal: If necessary, use clippers instead of razors to prevent microabrasions.
Prophylactic Antibiotics
Administering prophylactic antibiotics is a cornerstone of infection prevention. Guidelines recommend:
- Administering a single dose of a broad-spectrum antibiotic, such as cefazolin, within 60 minutes before the incision.
- Considering additional doses for prolonged surgeries or significant blood loss.
Patient Optimization
- Smoking Cessation: Encouraging patients to stop smoking at least four weeks before surgery.
- Glycemic Control: Ensuring blood glucose levels are well-managed in diabetic patients.
- Weight Management: Advising weight loss if appropriate to reduce surgical complications.
Intraoperative Measures for Infection Control
Maintaining a Sterile Environment
Adherence to strict aseptic techniques is essential during surgery. Key measures include:
- Using sterile instruments and equipment.
- Limiting the number of personnel in the operating room to minimize contamination.
- Maintaining proper ventilation systems to reduce airborne pathogens.
Surgical Technique
- Minimizing tissue trauma through precise surgical techniques.
- Using wound protectors to shield the incision site from contamination.
- Ensuring meticulous hemostasis to reduce hematoma formation, which can harbor bacteria.
Temperature Regulation
Maintaining normothermia during surgery has been shown to reduce infection rates. Strategies include:
- Using warming blankets or devices to stabilize body temperature.
- Monitoring core temperature throughout the procedure.
Postoperative Infection Prevention
Wound Care
Proper wound management is vital for preventing SSIs. Recommended practices include:
- Regularly inspecting the incision site for signs of infection, such as redness, swelling, or discharge.
- Keeping the wound clean and dry.
- Educating patients on proper wound care techniques and signs of infection to report.
Early Mobilization
Encouraging early ambulation helps improve circulation, reduce venous stasis, and lower the risk of complications such as deep vein thrombosis (DVT) and pulmonary embolism.
Catheter Management
- Removing urinary catheters as soon as possible to minimize UTI risks.
- Ensuring proper hygiene and care during catheter use.
Nutritional Support
Promoting adequate nutrition aids in healing and boosts immune function. Recommendations include:
- A diet rich in protein, vitamins, and minerals.
- Considering supplements for patients with deficiencies.
Recognizing and Managing Postoperative Infections
Early Signs of Infection
- Fever or chills.
- Increased pain or tenderness at the incision site.
- Foul-smelling or purulent wound discharge.
- Unusual fatigue or malaise.
Diagnostic Steps
- Blood tests to detect elevated white blood cell counts.
- Imaging studies, such as ultrasound or CT scans, to identify abscesses or deep infections.
- Microbial cultures to determine the causative organism and guide targeted antibiotic therapy.
Treatment Approaches
- Antibiotics: Tailored to the specific pathogen identified.
- Drainage Procedures: For abscesses or infected fluid collections.
- Surgical Debridement: In cases of severe or necrotizing infections.
Long-term Strategies for Infection Reduction
Quality Improvement Programs
Healthcare institutions should implement infection control programs that include:
- Regular audits and feedback on surgical outcomes.
- Ongoing education and training for surgical teams.
- Development and adherence to evidence-based protocols.
Patient Education
Empowering patients with knowledge about infection prevention can significantly enhance outcomes. Key topics include:
- The importance of adhering to follow-up appointments.
- Recognizing early signs of infection.
- Maintaining a healthy lifestyle to support recovery.
Preventing infections after an abdominal hysterectomy requires a comprehensive, multidisciplinary approach. By implementing evidence-based practices at every stage of care—from preoperative preparation to postoperative management—healthcare providers can significantly reduce infection rates, improve patient outcomes, and enhance overall quality of care.