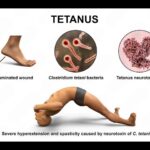
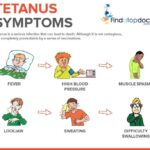
Tetanus, caused by Clostridium tetani, leads to a life-threatening neurological syndrome marked by severe muscle spasms and autonomic dysfunction. While immunization and wound care remain central to prevention, effective recovery hinges on adjunctive treatments that mitigate symptoms, neutralize toxins, and support physiological stability. A multidisciplinary approach, integrating pharmacological, supportive, and intensive care strategies, forms the backbone of modern tetanus adjunct treatment protocols.
Toxin Neutralization: Immediate Administration of Tetanus Immune Globulin (TIG)
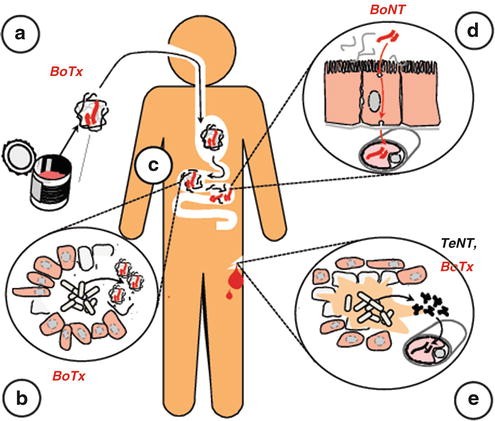
The cornerstone of adjunctive management is neutralizing unbound tetanospasmin, which continues to circulate in early stages.
Key Aspects:
- TIG Dose: 3000 to 6000 IU intramuscularly
- Mechanism: Binds and neutralizes unbound toxin before it enters the CNS
- Alternative: Intrathecal TIG (especially in severe cases), though not universally practiced
This intervention does not reverse existing symptoms but is crucial in halting progression.
Antibiotic Therapy: Eradicating Clostridium tetani at the Source
Eliminating the source of ongoing toxin production requires targeted antibiotic therapy.
Preferred Agents:
- Metronidazole (500 mg IV every 6–8 hours): First-line due to superior anaerobic coverage and lower neurotoxicity
- Penicillin G: An alternative, although associated with GABA antagonism, potentially worsening spasms
Additional Considerations:
- Antibiotic therapy typically extends for 7–10 days
- Local wound debridement must accompany antimicrobial use for optimal effect
Sedation and Neuromuscular Control: Preventing Spasms and Respiratory Compromise
Tetanus is characterized by painful and violent muscle contractions. Effective sedation and spasm control are imperative.
First-Line Muscle Relaxants:
- Benzodiazepines (Diazepam or Midazolam): Act as GABA agonists to reduce spasticity
- Dosing: Titrated based on severity, often requiring high continuous infusion in ICU
Adjunct Muscle Modulators:
- Baclofen (Intrathecal for severe cases): Targets spinal cord inhibition directly
- Dantrolene: Used selectively to reduce excitation-contraction coupling in muscles
In refractory cases, neuromuscular blockade using vecuronium or pancuronium, with mechanical ventilation, is warranted.
Autonomic Stabilization: Managing Cardiovascular Instability
Tetanus often results in autonomic dysfunction, manifesting as labile blood pressure, tachycardia, and arrhythmias.
Management Strategies:
- Beta-blockers (Labetalol, Esmolol): Control sympathetic overdrive
- Magnesium sulfate: Dual role in reducing spasms and stabilizing autonomic function
- Clonidine or dexmedetomidine: Central sympatholytic agents for severe dysautonomia
Close ICU monitoring is essential due to the unpredictability and rapid progression of symptoms.
Nutrition, Hydration, and Supportive Care in ICU Settings
Patients with tetanus often endure prolonged ICU stays, requiring meticulous supportive management.
Nutritional Support:
- High-caloric, high-protein diets, preferably via enteral feeding, support muscle repair and immune response
- Nasogastric or percutaneous feeding tubes used in case of trismus or intubation
Ventilatory Support:
- Indicated in moderate to severe cases with respiratory compromise or under neuromuscular blockade
- Weaning is gradual as spasms and autonomic instability subside
Pain and Environmental Management:
- Low-stimulus environments reduce the risk of triggering spasms
- Analgesics like morphine may be administered carefully alongside sedatives
Special Considerations: Pediatric and Neonatal Tetanus
Children and neonates require weight-adjusted doses of TIG, antibiotics, and sedatives. Neonatal tetanus, often fatal without intervention, demands early administration of TIG, intensive respiratory support, and maternal immunization as a preventive measure.
Emerging Therapies and Research Directions
Intrathecal TIG:
Shows promise in improving mortality outcomes, particularly in resource-limited settings where systemic delivery may be inadequate.
Monoclonal Antibodies:
Under development to target tetanospasmin with higher specificity and fewer systemic effects.
AI-Guided ICU Monitoring:
Advanced algorithms are being integrated into ICU settings for real-time analysis of autonomic fluctuations, optimizing medication titration and early detection of deterioration.
Effective management of tetanus extends beyond antitoxin administration to include a comprehensive adjunct treatment plan addressing infection, neurological symptoms, autonomic imbalance, and systemic needs. Timely intervention in a well-equipped intensive care environment ensures the best chance of survival and recovery. With vigilant care and integrated strategies, the burden of tetanus can be significantly reduced, even in severe presentations.