Tenosynovial Giant Cell Tumor (TGCT) is a rare, typically benign tumor that arises from the synovium—the thin layer of tissue lining joints, bursae, and tendon sheaths. It is characterized by proliferation of synovial-like cells, leading to mass formation and joint damage. TGCT most commonly affects the knee, ankle, hip, and fingers, and is divided into two clinical subtypes: localized and diffuse.
TGCT Subtypes
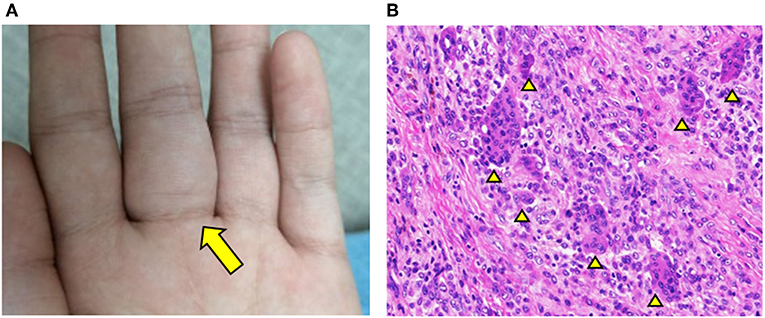
- Localized TGCT (L-TGCT): Affects small joints, especially the fingers and hands; also referred to as giant cell tumor of the tendon sheath.
- Diffuse TGCT (D-TGCT): Involves larger joints, predominantly the knee or hip; synonymous with pigmented villonodular synovitis (PVNS).
Pathophysiology and Etiology
TGCT is driven by a genetic alteration involving the CSF1 gene (colony-stimulating factor 1). In most cases, a chromosomal translocation causes overexpression of CSF1, which in turn attracts macrophages and other inflammatory cells, resulting in the formation of a tumor-like mass.
Though benign, TGCT can behave aggressively, especially in its diffuse form, causing joint destruction, bone erosion, and significant functional impairment.
Epidemiology and Risk Factors
- Incidence: Approximately 1.8 cases per million people annually for diffuse TGCT; localized forms are more frequent.
- Age Range: Most common in adults aged 30–50 years.
- Gender: Slight female predominance.
- Risk Factors:
- No definitive environmental or lifestyle risk factors identified.
- Genetic mutations in the CSF1 gene remain the primary driver.
Clinical Presentation of TGCT
Localized TGCT
- Gradual onset of painless swelling
- Often affects the fingers and hand tendons
- May restrict tendon movement over time
Diffuse TGCT
- Progressive joint pain, stiffness, and swelling
- Recurrent joint effusion
- Reduced range of motion
- Possible locking or catching sensation in the joint
- In advanced cases: joint instability and bone erosion
Diagnostic Evaluation
1. Physical Examination
Initial findings may include joint swelling, palpable mass, decreased mobility, or localized tenderness.
2. Magnetic Resonance Imaging (MRI)
- Gold standard for diagnosis
- Reveals lobulated mass, joint effusion, and hemosiderin deposits (low signal intensity on T2-weighted images)
- Differentiates between localized and diffuse types
3. Ultrasound
- May help assess superficial localized TGCT
- Visualizes hypoechoic mass adjacent to tendon sheaths
4. Histopathological Examination
- Confirms diagnosis via biopsy or surgical specimen
- Shows multinucleated giant cells, foam cells, fibrous stroma, and hemosiderin deposition
5. X-Rays and CT Scans
- May show bone erosion or joint space narrowing in diffuse cases
Differential Diagnoses
- Synovial sarcoma
- Hemophilic arthropathy
- Rheumatoid arthritis
- Lipoma arborescens
- Ganglion cyst
- Synovial chondromatosis
Treatment Options for Tenosynovial Giant Cell Tumor
1. Surgical Resection
- Primary treatment for both types
- Localized TGCT: Complete excision typically curative
- Diffuse TGCT: More complex due to extensive tissue involvement
- Open or arthroscopic synovectomy
- Higher risk of recurrence in diffuse forms
2. Radiation Therapy
- Used as adjunctive therapy in diffuse TGCT when complete resection is not possible
- Includes external beam radiotherapy and radiosynovectomy
- Helps reduce recurrence rate
3. Targeted Therapy
- Based on inhibition of CSF1 pathway
- Pexidartinib (TURALIO): First FDA-approved oral CSF1R inhibitor
- Indicated for adults with symptomatic, inoperable diffuse TGCT
- Requires liver function monitoring due to risk of hepatotoxicity
4. Observation
- In asymptomatic or slow-growing cases, especially in older adults
- Regular imaging follow-up is essential
Recurrence and Prognosis
- Localized TGCT: Low recurrence rate (~10–20%) post-complete excision
- Diffuse TGCT: High recurrence rate (up to 40–50%) without adjuvant therapy
- Prognosis:
- Excellent for localized forms
- Diffuse cases can be functionally debilitating if not properly managed
- Early diagnosis and multidisciplinary treatment significantly improve outcomes
Postoperative Rehabilitation and Monitoring
- Physical therapy to restore joint function and strength
- Regular MRI follow-ups to monitor for recurrence, especially within the first 2 years
- Long-term surveillance in diffuse cases to manage any residual disease
Frequently Asked Questions:
Is TGCT cancerous?
TGCT is considered a benign tumor, but diffuse TGCT can behave aggressively and damage surrounding structures.
Can TGCT come back after surgery?
Yes. Diffuse TGCT has a higher recurrence rate. Regular imaging and follow-up are critical post-treatment.
What is the success rate of TGCT treatment?
Localized TGCT has a high success rate after complete excision. Diffuse TGCT may require combination therapy for optimal outcomes.
How long does it take to recover from TGCT surgery?
Recovery time varies by location and extent of surgery. Localized excision may heal in a few weeks, while diffuse resection could take several months.
Are there non-surgical treatments for TGCT?
Yes. Targeted therapies like pexidartinib and radiotherapy are options when surgery is not feasible or recurrence occurs.
Tenosynovial Giant Cell Tumor is a unique and rare joint tumor requiring prompt diagnosis and specialized management. While localized forms are effectively treated with surgical excision, diffuse variants necessitate a multidisciplinary approach involving surgery, radiation, and targeted therapies. Advances in molecular therapy, especially CSF1R inhibitors, offer promising alternatives for patients with inoperable or recurrent disease. Early intervention remains the key to preserving joint function and improving long-term outcomes.

