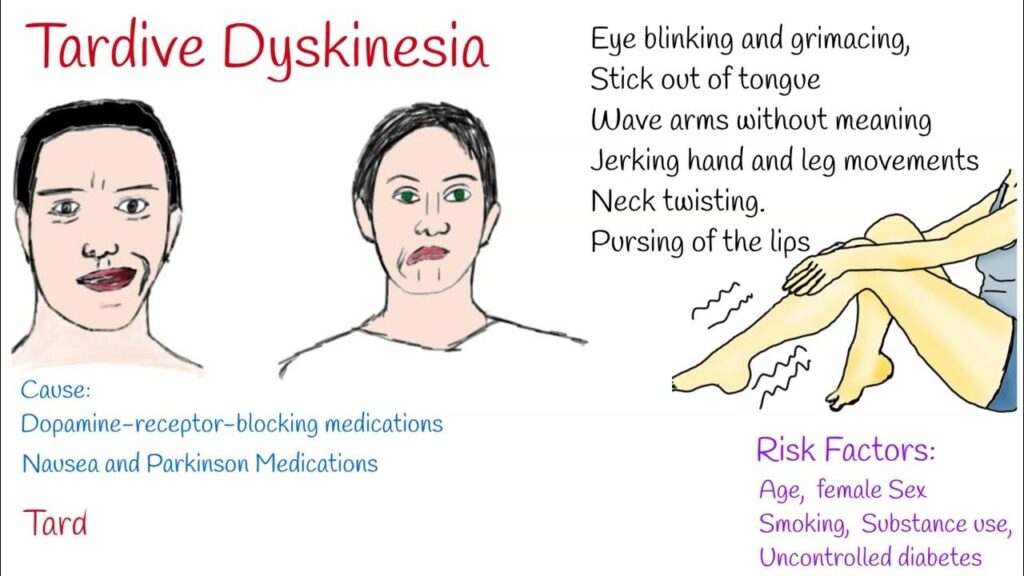
Tardive dyskinesia (TD) is a chronic, often irreversible neurological condition characterized by involuntary, repetitive movements. These movements typically affect the face, lips, tongue, trunk, and limbs. TD is most frequently associated with long-term use of dopamine receptor-blocking agents, particularly antipsychotic medications used to treat schizophrenia, bipolar disorder, and other psychiatric conditions.
Causes and Risk Factors of Tardive Dyskinesia
Primary Cause: Dopamine Receptor Blockade
Tardive dyskinesia primarily results from prolonged exposure to first-generation (typical) and second-generation (atypical) antipsychotics. These drugs block dopamine D2 receptors in the brain, leading to compensatory changes in receptor sensitivity and neural circuitry that result in involuntary movements.
Contributing Factors
- Duration of exposure: Longer treatment periods increase the risk
- High dosages of dopamine-blocking agents
- Older age
- Female sex
- History of mood disorders
- Presence of diabetes mellitus
- Genetic susceptibility (e.g., CYP2D6 polymorphisms)
Recognizing the Symptoms of Tardive Dyskinesia
Tardive dyskinesia symptoms may vary in intensity and presentation, often worsening over time. The most common manifestations include:
Orofacial Movements
- Lip smacking, puckering, or pursing
- Tongue protrusion or writhing
- Chewing motions without food
- Facial grimacing
Limb and Trunk Movements
- Rapid, jerky arm or leg movements
- Finger wiggling or tapping
- Shoulder shrugging
- Hip twisting or rocking
Respiratory and Vocal Effects
- Grunting or moaning
- Irregular breathing patterns
- Throat clearing or unusual vocalizations
Symptoms often intensify during stress and diminish during purposeful voluntary movements.
Differential Diagnosis: Conditions to Rule Out
Before diagnosing TD, clinicians must differentiate it from other movement disorders:
- Parkinson’s disease
- Huntington’s disease
- Tourette syndrome
- Dystonia
- Akathisia
- Essential tremor
Comprehensive clinical history and physical examination, combined with targeted neurological assessments, are essential to rule out these conditions.
Diagnostic Approach for Tardive Dyskinesia
Clinical Assessment
TD diagnosis is primarily clinical, based on history of antipsychotic use and symptom observation. Key steps include:
- Detailed medication history
- Neurological evaluation
- Movement pattern analysis
Standardized Rating Scales
- Abnormal Involuntary Movement Scale (AIMS): Most widely used tool to assess TD severity and monitor progression.
- DISCUS (Dyskinesia Identification System: Condensed User Scale): Useful for screening in clinical settings.
Diagnostic Criteria
- History of dopamine-blocking medication use for at least a few months
- Presence of involuntary movements lasting at least a month
- Exclusion of other movement disorders or underlying neurological conditions
Current Treatment Options for Tardive Dyskinesia
Discontinuation or Adjustment of Offending Agent
- Gradual reduction or substitution with lower-risk antipsychotics (e.g., clozapine or quetiapine) can mitigate symptoms.
- Abrupt discontinuation is discouraged due to potential psychiatric destabilization.
FDA-Approved Medications
Valbenazine (Ingrezza)
- First drug approved specifically for TD
- VMAT2 inhibitor: modulates dopamine release
- Administered once daily; minimal sedation or extrapyramidal effects
Deutetrabenazine (Austedo)
- VMAT2 inhibitor with slower metabolism
- Effective for both TD and chorea in Huntington’s disease
- Requires twice-daily dosing
Adjunctive Therapies
- Benzodiazepines (e.g., clonazepam): temporary relief but risk of dependency
- Ginkgo biloba extract: modest benefit in some clinical trials
- Vitamin E, melatonin, and omega-3 fatty acids: proposed antioxidants with limited clinical evidence
Non-Pharmacological Interventions
- Cognitive Behavioral Therapy (CBT): helps patients cope with psychosocial impact
- Physical therapy: aids in managing gait and limb dyskinesias
- Deep brain stimulation (DBS): considered in refractory, disabling TD cases
Long-Term Management and Prognosis
Tardive dyskinesia is often persistent, even after discontinuation of the causative agent. Management focuses on symptom control, minimizing functional impairment, and regular reassessment of antipsychotic necessity.
Monitoring
- Regular AIMS assessments during antipsychotic therapy
- Comprehensive review of medication regimens every 6–12 months
- Close observation for symptom progression or remission
Prognostic Factors
- Early detection and intervention correlate with improved outcomes
- Younger patients and those with mild symptoms show better recovery
- Chronic, untreated TD may lead to permanent disability and social isolation
Preventive Strategies for Tardive Dyskinesia
Risk Mitigation During Antipsychotic Therapy
- Use lowest effective dose for the shortest possible duration
- Prefer atypical antipsychotics with lower TD risk
- Implement drug holidays only when clinically appropriate
Regular Screening and Monitoring
- Conduct baseline AIMS assessments before initiating treatment
- Reassess every 3–6 months, particularly in high-risk patients
- Educate patients on early signs of TD and encourage prompt reporting
Personalized Medicine Approaches
- Pharmacogenetic testing to identify CYP2D6 or DRD2 polymorphisms
- Tailor antipsychotic choices and dosages based on individual metabolic profiles
Frequently Asked Questions:
What is the main cause of tardive dyskinesia?
Tardive dyskinesia is mainly caused by long-term use of dopamine receptor-blocking drugs, particularly antipsychotics.
Is tardive dyskinesia reversible?
TD may be reversible in some cases, especially with early intervention. However, it is often persistent and requires long-term management.
How is tardive dyskinesia diagnosed?
Diagnosis is clinical, supported by tools like the AIMS scale and based on history of medication use and movement observations.
Are there treatments for tardive dyskinesia?
Yes, valbenazine and deutetrabenazine are FDA-approved treatments. Adjusting medications and supportive therapies are also beneficial.
Can tardive dyskinesia be prevented?
Prevention involves judicious use of antipsychotics, regular monitoring, and using the lowest effective dose for the shortest duration.
Tardive dyskinesia is a serious and often lifelong movement disorder arising from prolonged use of dopamine-blocking medications. Early identification, regular monitoring, and timely intervention are key to reducing its burden. With advancements in targeted treatments and preventive strategies, healthcare providers can significantly improve the quality of life for patients affected by TD.

