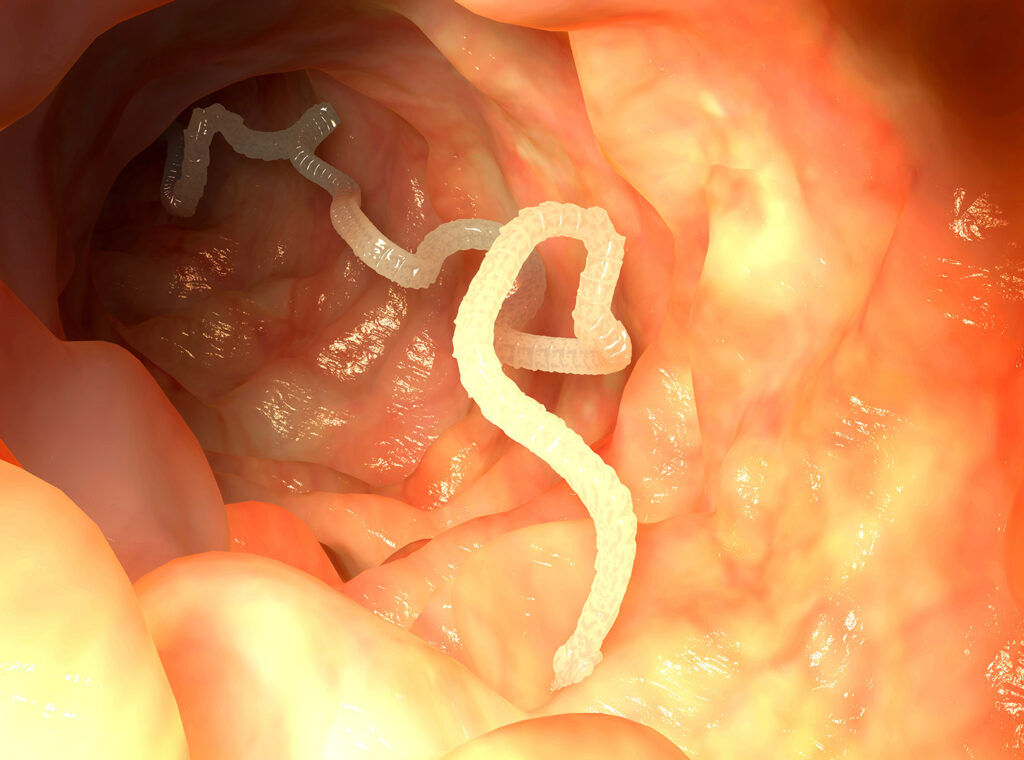
Taenia infection, clinically referred to as taeniasis, is a parasitic disease caused by the ingestion of Taenia species, primarily Taenia solium (pork tapeworm) and Taenia saginata (beef tapeworm). Infections occur globally, with higher prevalence in regions where sanitation is poor and raw or undercooked meat consumption is common. While often asymptomatic, Taenia infections can lead to severe complications such as neurocysticercosis, particularly with T. solium.
Causative Species of Taenia
Taenia solium
- Host: Humans (definitive), pigs (intermediate)
- Transmission: Ingestion of undercooked pork containing larval cysts (cysticerci)
- Complication: Can cause cysticercosis, especially when eggs are ingested
Taenia saginata
- Host: Humans (definitive), cattle (intermediate)
- Transmission: Ingestion of undercooked beef containing cysticerci
- Complication: Does not cause cysticercosis
Taenia asiatica
- Found primarily in Southeast Asia
- Lifecycle similar to T. saginata, but intermediate host is pigs
Lifecycle of Taenia Species
Understanding the lifecycle of Taenia is critical for grasping the infection route and intervention points.
This cycle perpetuates when humans consume infected meat without proper cooking.
Modes of Transmission
- Ingestion of undercooked or raw pork/beef containing viable cysticerci
- Fecal-oral transmission of eggs from human carriers, particularly dangerous with T. solium
- Contaminated water or food, especially in regions with open defecation
- Autoinfection in the case of T. solium, when eggs from feces are ingested by the same host, leading to cysticercosis
Symptoms and Clinical Manifestations
Taeniasis (Intestinal Infection)
- Often asymptomatic
- Nonspecific gastrointestinal symptoms:
- Abdominal discomfort
- Nausea
- Diarrhea or constipation
- Weight loss
- Visible passage of proglottids in stool
Cysticercosis (Larval Tissue Infection)
- Occurs when T. solium eggs are ingested
- Larvae invade tissues forming cysts in:
- Muscles
- Eyes
- Central nervous system (CNS)
Neurocysticercosis
- Major cause of acquired epilepsy in endemic areas
- Symptoms include:
- Seizures
- Headaches
- Hydrocephalus
- Neurological deficits
Diagnostic Methods for Taenia Infection
Stool Examination
- Detection of eggs or proglottids via microscopy
- Requires multiple stool samples for accurate diagnosis
Serological Tests
- Enzyme-linked immunoelectrotransfer blot (EITB) for detecting T. solium antibodies
- Used primarily in cysticercosis cases
Imaging
- CT or MRI scans crucial in diagnosing neurocysticercosis
- Visualizes cysts in brain tissues
Molecular Testing
- PCR assays provide species-specific identification
- Beneficial in distinguishing T. solium from T. saginata
Treatment Options for Taenia Infection
Antiparasitic Medications
- Praziquantel (5–10 mg/kg orally once) – first-line for intestinal taeniasis
- Niclosamide – effective but less commonly used
For Neurocysticercosis
- Albendazole (15 mg/kg/day for 8–30 days)
- Corticosteroids (e.g., dexamethasone) to reduce inflammation
- Antiepileptic drugs for seizure control
- Surgical intervention may be required for hydrocephalus or large cysts
Prevention Strategies
Meat Inspection and Cooking
- Cook pork and beef to at least 63°C (145°F)
- Avoid raw or undercooked meat consumption
- Freeze meat at −10°C for several days to kill cysticerci
Sanitation and Hygiene
- Practice proper handwashing, especially after defecation
- Prevent open defecation near livestock areas
- Improve sanitation infrastructure
Public Health Education
- Educate communities in endemic regions about:
- Safe cooking practices
- Personal hygiene
- Risks of fecal contamination
Livestock Management
- Regular veterinary checks
- Avoid feeding livestock with untreated human waste
- Vaccination of pigs (e.g., TSOL18 vaccine) in endemic regions
Global Epidemiology and Public Health Impact
Taenia infections remain a major public health issue in many developing countries, especially in Latin America, Sub-Saharan Africa, and Asia. The World Health Organization (WHO) considers neurocysticercosis a leading cause of preventable epilepsy.
Prevalence rates are closely linked to:
- Cultural dietary habits
- Socioeconomic conditions
- Access to healthcare
Efforts toward One Health approaches, integrating human, animal, and environmental health, are key to controlling transmission.
Summary Table: Key Differences Between T. solium and T. saginata
| Feature | Taenia solium | Taenia saginata |
|---|---|---|
| Intermediate Host | Pig | Cattle |
| Human Complication | Cysticercosis | None |
| Proglottid Motility | Less active | Highly motile |
| Length | 2–7 meters | Up to 10 meters |
| Diagnostic Features | Armed scolex | Unarmed scolex |
| Geographic Prevalence | Asia, Africa, Latin Am. | Africa, Latin Am., Asia |
Frequently Asked Questions:
What is Taenia infection?
It is a parasitic disease caused by ingestion of tapeworms, typically T. solium or T. saginata, via raw or undercooked meat.
Can Taenia cause brain infection?
Yes, T. solium eggs can cause neurocysticercosis, a serious brain infection resulting in seizures and other neurological symptoms.
How is Taenia infection diagnosed?
Diagnosis involves stool tests, imaging, and serological assays, depending on whether the infection is intestinal or tissue-based.
Is taeniasis contagious?
Human-to-human transmission occurs only with T. solium eggs, which can contaminate food or water through poor hygiene.
How can Taenia infections be prevented?
Prevention involves proper cooking of meat, improved sanitation, hand hygiene, and public health education.
Taenia infection is a preventable parasitic disease with significant health implications, particularly in low-resource settings. Comprehensive measures—including diagnosis, treatment, and community-level interventions—are essential for controlling transmission and minimizing complications. Awareness, combined with improved food safety and sanitation, remains the cornerstone of effective prevention.