Systemic mastocytosis (SM) is a rare and complex condition characterized by the abnormal accumulation and proliferation of mast cells in various tissues throughout the body, leading to a wide range of symptoms. These mast cells, typically involved in allergic reactions, become dysfunctional in SM, resulting in excessive release of histamine and other mediators that trigger inflammatory responses. While systemic mastocytosis can occur in individuals of any age, it is most commonly diagnosed in adults.

Key Features of Systemic Mastocytosis
- Abnormal mast cell proliferation: An increase in mast cells in organs such as the skin, liver, spleen, and bone marrow.
- Histamine release: Excessive histamine causes symptoms similar to allergic reactions.
- Chronic condition: Systemic mastocytosis can lead to long-term health issues if not managed appropriately.
Pathophysiology of Systemic Mastocytosis
Mast cells are an integral part of the immune system and play a key role in allergic responses. They contain various chemical mediators, including histamine, heparin, and cytokines. In systemic mastocytosis, genetic mutations, most commonly involving the KIT gene, cause mast cells to proliferate uncontrollably. This excessive proliferation of mast cells can occur in various organs and tissues, leading to symptoms ranging from skin lesions to gastrointestinal distress.
The KIT mutation is particularly significant as it results in abnormal mast cell function. Mutations in this gene can lead to the uncontrolled growth of mast cells, which accumulate in different parts of the body, often resulting in organ damage and systemic symptoms.
Symptoms of Systemic Mastocytosis
Cutaneous Symptoms
The most visible symptoms of systemic mastocytosis are skin-related. Urticaria pigmentosa, a type of cutaneous mastocytosis, is characterized by brownish patches or bumps on the skin that may become itchy when rubbed. These skin lesions can sometimes cause dermographism, a condition where raised red welts appear on the skin when scratched.
Gastrointestinal Symptoms
Mast cell proliferation can affect the gastrointestinal (GI) tract, leading to a range of symptoms, including:
- Abdominal pain: Often chronic and associated with bloating.
- Diarrhea: Frequent episodes can occur due to histamine release in the gut.
- Nausea and vomiting: Resulting from mast cell activation in the GI tract.
Anaphylaxis and Other Allergic Reactions
One of the most serious aspects of systemic mastocytosis is the potential for anaphylactic reactions. The overproduction of histamine can cause severe allergic reactions, even in the absence of external allergens. Symptoms of anaphylaxis may include:
- Swelling of the throat
- Difficulty breathing
- Rapid drop in blood pressure
Bone Pain and Fatigue
Mast cell infiltration in the bone marrow and other tissues can cause bone pain, fatigue, and a feeling of general malaise. These symptoms are typically associated with more advanced stages of systemic mastocytosis.
Cardiovascular Symptoms
Patients with systemic mastocytosis may experience flushing, tachycardia (increased heart rate), and low blood pressure, especially after mast cell activation. These cardiovascular symptoms result from the widespread release of histamine and other inflammatory mediators.
Diagnosis of Systemic Mastocytosis
Clinical Evaluation and Symptoms
Diagnosis of systemic mastocytosis begins with a thorough clinical evaluation. A detailed history of symptoms and family history of mast cell diseases is essential. The presence of skin lesions like urticaria pigmentosa and gastrointestinal symptoms can suggest the possibility of systemic mastocytosis.
Laboratory Tests
- Serum tryptase levels: Elevated levels of tryptase, an enzyme released by mast cells, can indicate mast cell activation and are a key marker for systemic mastocytosis.
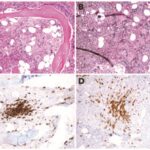
- Bone marrow biopsy: This is a definitive diagnostic test, as it reveals the infiltration of mast cells in the bone marrow.
- KIT mutation analysis: A genetic test that identifies mutations in the KIT gene, which are often present in systemic mastocytosis.
- Urinary histamine metabolites: Elevated levels of N-methylhistamine and other histamine metabolites can support the diagnosis.
Imaging
In some cases, imaging studies such as ultrasound or CT scans may be used to assess organ involvement, especially in cases where mast cell proliferation is suspected in the liver, spleen, or gastrointestinal tract.
Treatment Options for Systemic Mastocytosis
First-Line Treatment: Antihistamines
The cornerstone of treatment for systemic mastocytosis involves managing the symptoms caused by mast cell activation, particularly histamine release. Antihistamines are often prescribed to control allergic symptoms, such as skin rashes and itching. These medications block the effects of histamine and help alleviate symptoms like flushing, itching, and abdominal discomfort.
Mast Cell Stabilizers
Cromolyn sodium and other mast cell stabilizers work by preventing mast cells from releasing histamine and other inflammatory substances. These medications are typically used in conjunction with antihistamines to improve symptom control.
Tyrosine Kinase Inhibitors
For patients with advanced systemic mastocytosis or those who do not respond to conventional therapies, tyrosine kinase inhibitors (TKIs) such as midostaurin have shown promise. These medications target the mutated KIT protein that drives mast cell proliferation. TKIs can help reduce the number of mast cells and prevent the release of inflammatory mediators.
Corticosteroids
Corticosteroids like prednisone are sometimes used to reduce inflammation and treat severe symptoms. However, their use is generally limited due to potential side effects when used long-term.
Chemotherapy and Stem Cell Transplantation
In rare, more severe cases of systemic mastocytosis, particularly when it progresses to mast cell leukemia or when organs become severely damaged, chemotherapy or stem cell transplantation may be considered. These treatments aim to reduce the number of mast cells and prevent further organ damage.
Prognosis and Long-Term Outlook
The prognosis of systemic mastocytosis varies depending on the extent of mast cell involvement and the presence of associated malignancies like mast cell leukemia. Most patients with indolent (mild) systemic mastocytosis can manage their symptoms with antihistamines and mast cell stabilizers, leading to a relatively normal quality of life.
However, for those with aggressive forms of the disease, especially those with bone marrow involvement or organ dysfunction, the prognosis may be less favorable. Early detection and treatment are crucial to preventing complications and improving long-term outcomes.
Lifestyle and Monitoring Strategies for Systemic Mastocytosis
Avoiding Triggers
Patients with systemic mastocytosis should identify and avoid triggers that may cause mast cell activation. Common triggers include:
- Extremes in temperature
- Stress
- Certain foods or drinks (such as alcohol, vinegar, or fermented products)
- Infections
Regular Follow-up
Regular follow-up appointments are essential for monitoring disease progression and adjusting treatment plans. This may include periodic serum tryptase testing and other diagnostic evaluations to assess the effectiveness of the treatment regimen.
Frequently Asked Questions:
Q1: Can systemic mastocytosis be cured?
Currently, there is no cure for systemic mastocytosis, but symptoms can be managed effectively with medication.
Q2: How is systemic mastocytosis different from mast cell activation syndrome (MCAS)?
While both involve abnormal mast cell activation, systemic mastocytosis is a disease characterized by the abnormal proliferation of mast cells in various organs, while MCAS refers to the excessive activation of mast cells without the presence of significant mast cell accumulation.
Q3: Can systemic mastocytosis be inherited?
While some genetic mutations related to systemic mastocytosis can be inherited, most cases are sporadic, with no family history.
Q4: What is the role of KIT mutations in systemic mastocytosis?
KIT mutations are the most common genetic alteration in systemic mastocytosis, causing abnormal mast cell growth and the release of inflammatory mediators.
Q5: What lifestyle changes can help manage systemic mastocytosis?
Patients should avoid known triggers, manage stress, maintain a healthy diet, and stay vigilant for any new or worsening symptoms.