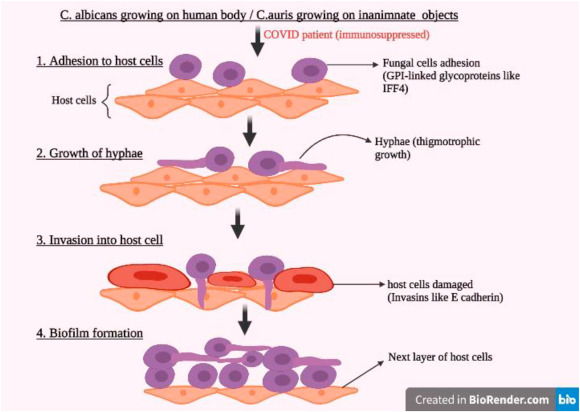
Systemic candidiasis, also referred to as invasive candidiasis, is a life-threatening fungal infection primarily caused by Candida species, most commonly Candida albicans, C. glabrata, C. parapsilosis, C. tropicalis, and the multidrug-resistant C. auris. It predominantly affects immunocompromised individuals, critically ill patients in intensive care units (ICUs), and those with central venous catheters or recent broad-spectrum antibiotic exposure.
Despite advancements in antifungal pharmacotherapy, mortality remains high—ranging from 30% to 60%—necessitating optimized strategies through adjunctive treatment modalities that enhance the efficacy of systemic antifungal agents, improve host immune responses, and reduce resistance development.
Primary Antifungal Therapies in Systemic Candidiasis
Echinocandins: First-Line Therapy
- Agents: Caspofungin, Micafungin, Anidulafungin
- Mechanism: Inhibit β-1,3-D-glucan synthesis in fungal cell walls
- Advantages: Fungicidal activity, low toxicity, minimal drug interactions
- Role in adjunct use: Preferred base therapy for combination with immune modulators
Azoles
- Agents: Fluconazole, Voriconazole, Posaconazole
- Effective against susceptible Candida strains
- Limitations: Increasing resistance, drug-drug interactions, hepatotoxicity
Polyenes
- Agent: Amphotericin B (liposomal formulations preferred)
- Broad-spectrum coverage but associated with nephrotoxicity
- Often used when resistance or intolerance to other agents is suspected
Rationale and Types of Adjunctive Treatments for Systemic Candidiasis
Adjunctive therapies are designed to work synergistically with primary antifungal agents to accelerate clearance, overcome host immune suppression, and improve overall survival.
Immunotherapy as an Adjunct in Systemic Candidiasis
Granulocyte Colony-Stimulating Factor (G-CSF) and GM-CSF
- Enhances neutrophil recovery and function
- Useful in neutropenic patients or bone marrow suppression
- Studies demonstrate improved outcomes when combined with antifungals
Interferon-Gamma (IFN-γ)
- Boosts Th1-mediated antifungal immune responses
- Promotes macrophage activation and fungicidal activity
- Particularly relevant in refractory or relapsing infections
Monoclonal Antibodies and Vaccine Candidates
- Anti-Candida antibodies (e.g., against β-glucan or Als3 proteins)
- Investigational use as adjunct immunotherapy
- NDV-3A vaccine: A promising candidate showing cross-protection against multiple Candida species
Source Control and Supportive Care in Adjunctive Management
Effective adjunctive treatment requires prompt identification and elimination of fungal reservoirs:
- Catheter removal: Mandatory in Candida bloodstream infections
- Surgical drainage: In cases of deep-seated abscesses or infected prosthetic material
- Hemodynamic stabilization: Through fluid resuscitation and vasopressor support in septic patients
- Parenteral nutrition optimization: Reduces gut colonization and translocation of Candida
Diagnostic Optimization as an Adjunctive Strategy
Accurate and early diagnosis is critical to initiating timely antifungal and adjunctive therapies.
Non-Culture Diagnostics
- β-D-glucan assay: Detects fungal cell wall components; high sensitivity
- Mannan/anti-mannan assays: Detects Candida cell wall polysaccharides and antibodies
- T2Candida Panel: Rapid molecular test providing species-level identification from whole blood within 3-5 hours
- PCR and next-generation sequencing (NGS): Useful in persistent or cryptic candidemia
Adjunctive diagnostics aid in distinguishing colonization from invasive disease, monitoring treatment response, and tailoring therapy.
Combination Antifungal Therapy as an Adjunctive Option
Though monotherapy remains the standard, combination therapy is considered in select scenarios:
- Echinocandin + Amphotericin B: For multidrug-resistant Candida (e.g., C. auris)
- Azole + Echinocandin: Potential synergistic effects, especially in deep-seated candidiasis
- Adjunct with Immunotherapy: To reinforce immune clearance alongside direct antifungal activity
Caution: Limited randomized controlled trials (RCTs); use reserved for salvage therapy or critically ill patients with high fungal burden.
Adjunctive Approaches in Neonatal and Pediatric Systemic Candidiasis
Neonates, especially those with very low birth weight, are highly vulnerable to invasive candidiasis. Adjunctive strategies in this population include:
- Early removal of central lines
- Empiric echinocandin therapy in high-risk settings
- Use of fluconazole prophylaxis in NICUs with high incidence
- Consideration of G-CSF in immunocompromised infants
Emerging adjuncts such as recombinant IFN-γ and fungal vaccines are under evaluation for pediatric use.
Antifungal Stewardship and Resistance Management
Adjunctive care in systemic candidiasis must also include antifungal stewardship:
- Minimize unnecessary exposure to azoles and polyenes
- Rapid de-escalation based on culture and sensitivity
- Surveillance of resistance patterns, especially for C. glabrata and C. auris
- Implement hospital-wide protocols to optimize antifungal use in ICUs and oncology units
Future Adjunctive Therapeutics Under Investigation
Host-Directed Therapies
- Modulation of innate immune checkpoints (e.g., Dectin-1, CARD9 pathway agonists)
- TLR-based immune modulators
Fungal Biofilm Disruption
- Anti-biofilm agents such as farnesol and DNase
- Targeting biofilm resistance mechanisms in catheter-related candidemia
Nanomedicine
- Liposomal delivery systems for enhanced drug penetration
- Antifungal-loaded nanoparticles for site-specific action with reduced toxicity
Frequently Asked Questions:
Q1. Why is adjunctive therapy necessary in systemic candidiasis?
Adjunctive therapies support antifungal efficacy by enhancing immune response, controlling infection sources, and improving diagnostic precision.
Q2. Can immunotherapy be used in all patients with systemic candidiasis?
No. Immunotherapy is reserved for immunocompromised or refractory cases and should be tailored based on individual risk-benefit assessments.
Q3. Is combination antifungal therapy superior to monotherapy?
Not routinely. Combination therapy may be beneficial in select cases with resistant strains or severe infection but lacks robust RCT support.
Q4. What are the most effective adjunctive diagnostics?
β-D-glucan assays, T2Candida panels, and PCR-based tools provide rapid and accurate diagnosis, crucial for early intervention.
Q5. Does removing catheters cure systemic candidiasis?
Catheter removal is critical but not curative alone. It must be coupled with systemic antifungal therapy and, where needed, adjuncts.