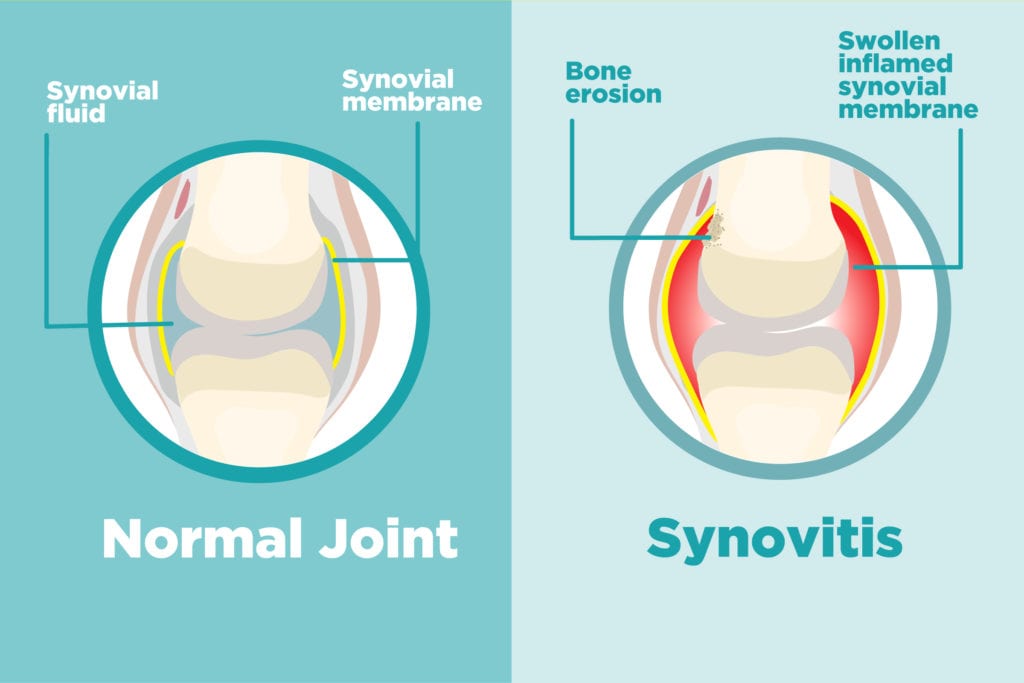
Synovitis due to osteoarthritis represents a secondary inflammatory process within the synovial membrane triggered by mechanical and biochemical degeneration of articular cartilage. While osteoarthritis (OA) has traditionally been viewed as a non-inflammatory joint disease, recent evidence highlights the pivotal role of low-grade synovial inflammation in symptom progression, joint dysfunction, and cartilage breakdown.
Synovitis amplifies the pain and swelling associated with OA and serves as both a marker of disease severity and a potential therapeutic target. Understanding its pathogenesis is essential to managing chronic symptoms and halting structural deterioration.
Anatomy of Synovial Inflammation in Osteoarthritis
The synovial membrane, lining the inner capsule of diarthrodial joints, responds to mechanical stress and debris from degenerated cartilage by initiating an inflammatory cascade. In OA-associated synovitis, macrophage activation and synoviocyte proliferation result in:
- Increased vascular permeability
- Immune cell infiltration
- Pro-inflammatory cytokine release (IL-1β, TNF-α)
- Elevated matrix metalloproteinases (MMPs)
These mediators perpetuate cartilage damage and pain signaling, contributing to the progressive cycle of degeneration.
Causes and Risk Factors of OA-Related Synovitis
While osteoarthritis is the primary driver, several compounding factors increase the likelihood and severity of synovitis:
- Mechanical stress from joint overuse or misalignment
- Cartilage matrix degradation products acting as immune stimuli
- Aging, which reduces repair capacity of both cartilage and synovium
- Obesity, which increases mechanical load and systemic inflammation
- Genetic predisposition to inflammatory responses in OA
- Prior joint injuries or surgeries, which accelerate synovial irritation
Clinical Presentation of Synovitis in Osteoarthritis
Patients with osteoarthritis and concurrent synovitis typically present with exacerbated symptoms compared to those with mechanical OA alone. Clinical features include:
- Persistent joint pain, worsened by activity
- Joint swelling due to synovial effusion
- Stiffness, especially after periods of inactivity
- Decreased range of motion
- Warmth and tenderness on palpation
The knee is the most frequently affected joint, but synovitis may also involve the hip, shoulder, and small joints of the hand in advanced OA.
Diagnostic Approach to Synovitis in OA Patients
1. Clinical Evaluation
- Palpable swelling and warmth
- Pain out of proportion to radiographic findings
- Fluctuance indicating joint effusion
2. Imaging Modalities
- Ultrasound: Identifies synovial thickening and effusion in real-time
- MRI: Gold standard for visualizing synovitis, bone marrow lesions, and cartilage status
- X-rays: Reveal osteophytes, joint space narrowing, and subchondral sclerosis but do not detect active inflammation
3. Laboratory Testing
- Synovial fluid analysis: Confirms non-infectious inflammation (mildly elevated WBCs, no crystals or pathogens)
- Serological markers: Typically absent or normal in primary OA; elevated CRP/ESR may be noted with significant synovitis
Impact of Synovitis on Osteoarthritis Progression
Synovitis is not merely a byproduct of OA but a key driver of disease progression. Chronic inflammation accelerates cartilage breakdown through enzymatic activity and disrupts the balance of cartilage synthesis and repair.
Key consequences include:
- Increased cartilage matrix degradation
- Higher rates of joint space loss
- Worsening pain severity and frequency
- Functional impairment and reduced quality of life
- Faster transition from early to late-stage OA
Therapeutic Strategies for Managing OA-Related Synovitis
1. Pharmacologic Interventions
- NSAIDs: First-line agents to reduce pain and synovial inflammation (e.g., naproxen, diclofenac)
- Intra-articular corticosteroids: Rapid relief of synovial inflammation in acute flares
- Hyaluronic acid injections: May reduce synovial irritation and improve joint lubrication
- Emerging biologics: Research on IL-1β and TNF-α inhibitors is ongoing for inflammatory OA
2. Physical Therapy and Rehabilitation
- Range-of-motion exercises to prevent stiffness
- Strength training to stabilize affected joints
- Aquatic therapy for low-impact conditioning
3. Weight Management and Lifestyle
- Weight reduction: Decreases mechanical load and inflammatory mediators
- Joint protection strategies: Ergonomic aids, orthotics, and modified activity patterns
4. Surgical Options
- Arthroscopic debridement: For mechanical symptoms with persistent synovitis, though benefit is limited in OA
- Total joint arthroplasty: Indicated in advanced OA with refractory pain and functional loss
Preventive Strategies and Long-Term Joint Health
To minimize the risk of recurrent or progressive synovitis in OA:
- Engage in regular low-impact exercise (e.g., swimming, cycling)
- Avoid prolonged joint overload or repetitive strain
- Address biomechanical abnormalities early (e.g., with physical therapy or bracing)
- Monitor symptom progression and seek early intervention during inflammatory flares
Frequently Asked Questions:
Q1. Can synovitis worsen osteoarthritis?
Yes, synovitis accelerates cartilage degradation and contributes to faster joint degeneration in OA.
Q2. Is synovitis in OA reversible?
While chronic synovitis may persist, early intervention can reduce inflammation and slow joint damage.
Q3. How is synovitis in osteoarthritis diagnosed?
Through clinical examination, imaging (particularly MRI or ultrasound), and synovial fluid analysis to rule out infection or crystals.
Q4. What is the most effective treatment for OA-related synovitis?
NSAIDs and intra-articular corticosteroids offer significant symptom relief; long-term control involves exercise, weight loss, and potentially surgery.
Q5. Does synovitis always occur with osteoarthritis?
No, not all OA patients develop synovitis, but those who do tend to have more severe symptoms and faster disease progression.